This piece was first posted on Substack. To comment, please go there.
Imagine the day you, the reader, get the COVID-19 vaccine. Think about what that day will look like. You will wake up in your home or apartment. You will shower. You will eat breakfast. You will get in your car, perhaps using your smartphone for directions to the vaccination site. Then you will go get the vaccine. Which of these activities will be most supportive of health? You might say getting the vaccine. But imagine what your day would be like if you got the vaccine, but took none of the other actions. Imagine you do not wake up in a home because you do not have one, or perhaps you have one but it lacks the reliable water and heating that allow you to shower and stay warm in winter. Imagine you skip breakfast because you have no food. Imagine you walk to the vaccination site (say, three or four miles) because you have no car. Imagine you spend an extra hour outside because you get lost without a smartphone to help you navigate. You get the shot, but how healthy can you really be, if you get it in such a context? Important as the vaccine is for you, it is clear that if your life continues to unfold amid such deprivation, it will not be healthy, and may not even continue very long.
Material resources, then, and the money that provides them, are central to health. This is why more nuanced discussions of the pandemic have been just as sensitive to the economic effects of COVID-19 as they have been to the viral threat. Anything that deepens material need in the US is just as challenging to health as the diseases we face. This is why the pandemic era has generated bipartisan support for the necessity of economic stimulus. It is why political figures as disparate as Mitt Romney and Andrew Yang have agreed on the importance of providing direct cash assistance to Americans. And it is why central to the Biden-Harris administration’s plan for addressing the pandemic is a $1.9 trillion economic rescue package. The plan is proposed to include $1,400 stimulus checks, rental assistance and an extended eviction moratorium, an extension of increased food stamp benefits, expanding the child care tax credit, subsidies for health insurance premiums, greater unemployment aid, more aid for small businesses, aid to state and local governments, and a $15 hourly minimum wage. It is a plan which approaches the level of ambition necessary to counter this crisis and lay the groundwork for a healthier, post-pandemic world.
Our approach to health is largely a matter of emphasis. There is so much that matters for health and so comparatively little energy and political capital devoted to large-scale structural shifts in the foundations of health. This is especially true for a fledgling administration, which must choose its priorities carefully, so as to maximize the good it can do, in a pre-midterms window of political opportunity. Given these realities, it is important to know what matters most for health, what interventions would make the most immediate difference in improving the health of the US population. So, what would make the most difference in our present moment? There is really no question here. The most difference can be made by policies which support getting Americans the material resources they need to be well. To have health, we need to have money, and the resources money buys. Ideally, we do not need to be rich, but we need enough for our basic needs to be met and a little extra for the peace of mind that comes with knowing we are covered in the event of emergencies. In the short-term, however, Americans need enough to make what is, for many, an impossible situation a little less hard. I do not just mean the situation of COVID-19. For many Americans, the pre-pandemic status quo was near enough to impossible to fall well short of sustaining a healthy life.
At the same time, the status quo has greatly benefited the well-off, whose health is supported by increasingly entrenched inequality which has created a country of health haves and have nots. We often hear this inequality characterized as the gap between the top one percent and everyone else. But the real traction is in the widening gap between the top 20 percent of earners and the lower 80 percent. I was recently on a research team which looked at this gap in terms of cardiovascular outcomes. The graph below is taken from our study. It shows that those in the top 20 percent were far less likely to suffer from poor cardiovascular outcomes than those in the bottom 80 percent, and that this disparity is growing. These outcomes are just one reflection of the many ways money, and the conditions of economic inequality, shape health.
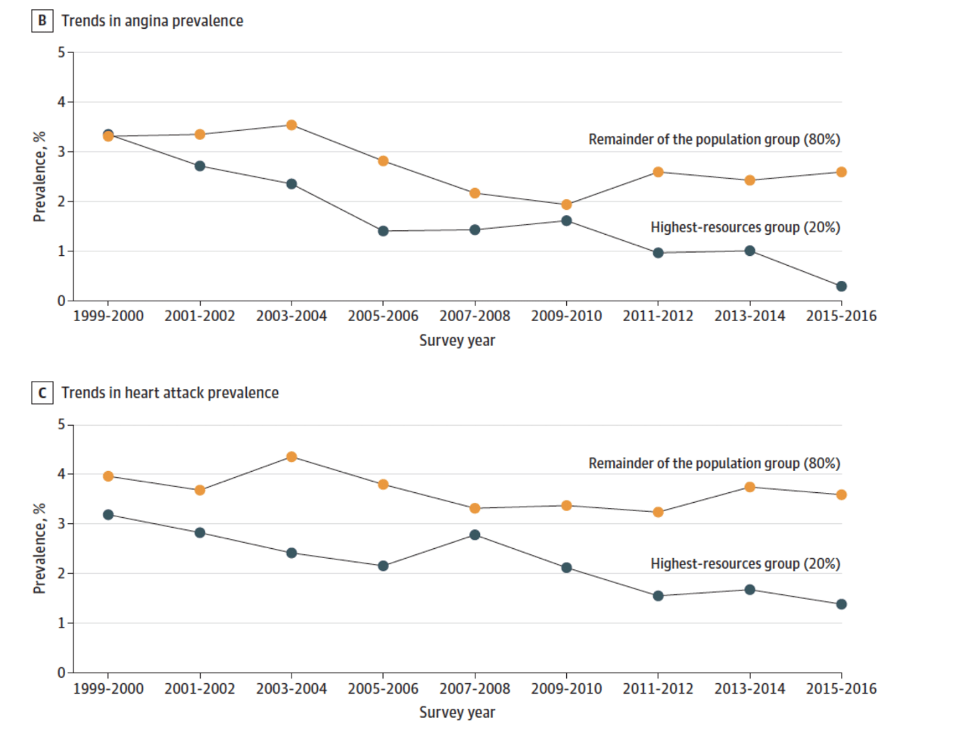
Source: Abdalla SM, Yu S, Galea S. Trends in Cardiovascular Disease Prevalence by Income Level in the United States. JAMA Network Open. 2020; 3(9): e2018150.
Now, in a free society, some inequality is inevitable, even healthy. But there comes a point where it becomes destabilizing, particularly when it is enabled by a system which creates extra advantages for those who already have much, allowing the wealthy to entrench their money and accumulate more, while ever-larger segments of society sink into a hole, with no lifelines forthcoming. This is what has been happening in the US, starting roughly during the Reagan administration, when a push for deregulation took hold at the federal level, resulting in rules which disproportionately benefit big business and the financial sector (or, more accurately, resulting in the dismantling of rules meant to reign in these sectors’ excesses) at the expense of middle-class and poor Americans. As a consequence, health for all but the well-off has suffered.
When the pandemic hit, the ongoing problem of inequality, and the intimate, kitchen table challenges of not having enough with which to get by, intersected with an unprecedented crisis, to deepen the country’s pain. Throughout the pandemic, lack of assets has been linked with greater risk of dying from COVID-19. It has worsened the pandemic’s effect on both physical and mental health. In another recent study, our team found prevalence of depression symptoms in the US rose more than three-fold during the pandemic, with individuals with fewer economic resources facing an even greater burden of depressive symptoms.
Fundamentally, these outcomes reflect that people do not have money to buy the resources they need to be healthy. The reasons they do not have money are just structural enough that we have a responsibility to do something about them at the federal level. The time to do so is now, with the 40-year emergency of an eroding American Dream intersecting with the 10-month crisis of a global pandemic. There are many visions for what doing something about this might mean. Some seek a limited stimulus, while some, on the farther end of the political spectrum, seek a more fundamental restructuring of our economic system. I would argue for us to engage with what is before us now—the recovery package—to make it as reflective as possible of what the country needs in this moment, to pass it with all possible speed, and to follow it up with more consistent material support in whatever form is most politically feasible, with an eye towards making such support a long-term feature of our system. This can be done pragmatically, and—as recent months have shown—with bipartisan support, though Democrats should not hesitate to use their slim majority to get this done, should Republican demands threaten either the integrity of the stimulus or the efficiency with which it might be passed. We have played the miser too long in the face of crushing collective need, and dressed this malpractice in a succession of ideological cloths over the years. At this transitional moment, it is time to try something new.
Finally, a word about this moment. The Trump administration got much wrong—in its pandemic response, and in its broader approach to governing. With last month’s political sea change, there is a temptation to try to right all these wrongs as quickly as possible, to throw as many solutions into the breach made by the last four years as we can—hence President Biden’s recent string of executive orders. This is understandable, admirable even, but it also runs the risk of suggesting all of these steps are of commensurate importance. The fact is they are not, particularly in the context of the emergency, so worsened by the pandemic, of American need. At the present moment, all solutions are not created equal. There are tradeoffs, in politics and in health. One of the hallmarks of our COVID-19 response has been our reluctance to acknowledge this. There have been loud calls to do everything that might address the pandemic, and all at once, with little consideration for the constraints of limited time and energy, and the ways in which doing everything at once can produce a level of incoherence and contradiction a national public health response, much less a presidency finding its feet, can ill-afford. Americans need the resources that support health as much as they need vaccines. We should be able to provide both, until the emergencies we face—COVID-19 and the worst effects of inequality—are well and truly behind us.
Sandro Galea, MD, DrPH, is Professor and Dean at the Boston University School of Public Health. His upcoming book, The Contagion Next Time, will be published in fall 2021. Subscribe to his weekly newsletter, The Healthiest Goldfish, or follow him on Twitter: @sandrogalea


