When I graduated from medical school in 2006, I was completely unaware there was a “preventive medicine” residency. Primary care was largely ignored by highly competitive students looking for the best salaries and lifestyles. The emphasis from mentors and peers was always on the “ROAD” to success: radiology, ophthalmology, anesthesiology and dermatology.
Outside of a single guest lecture I received from Dr. Dean Ornish during my second year, “prevention” as a field was minimized to vaccinations, mammograms and colon screenings… In other words, just those interventions that somehow triaged into a business model.
After recently attending the American College of Preventive Medicine’s 63rd annual conference in Portland, Oregon, I’m sorry to report the landscape is largely unchanged. Political and business concerns, chiefly in the form of poorly aligned reimbursement models, continue to reign as the decision-making framework that guides the future of the medical profession and patients’ lives. Physicians are still under the gun of dubious insurance practices, endless bureaucratic demands, and now a growing pool of unstructured data.
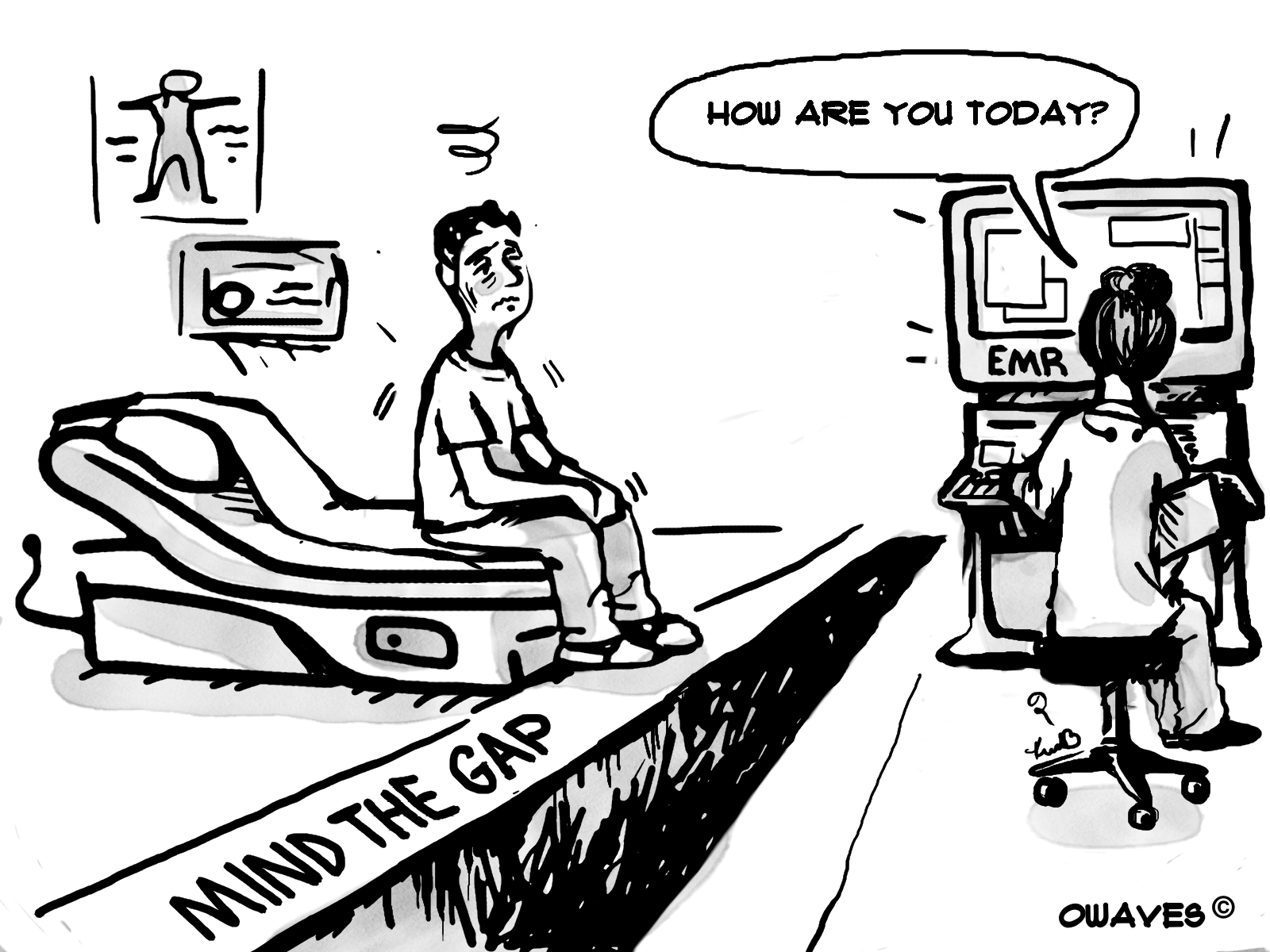
The most forward-thinking leaders of the group are calling for a focus on “outcomes” to guide reimbursement and policy models, rather than fee for service models of the past. While this is undoubtedly a positive next stage of our evolution as an industry, what strikes me as consistently missing from these discussions is any real focus on the patient-physician relationship. In the daily practice of healing, is there no room to explore the power of human-to-human interaction?
It seems to be regarded as a novelty, aside or lost cause… In the days of RVUs and number of patients seen per hour as core administrative policies driving hire and fire decisions… perhaps this is to be quietly accepted. And yet, I couldn’t help but feel there is a large hole in the room.