Bunions are one of the most common conditions presented to any foot and ankle surgeon, so it should be no surprise that bunion surgeries are an intricate part of their practices. Foot and ankle surgeons see bunions (also known as hallux valgus) daily and are intimately familiar with the treatment and surgical options.
However, as a patient, it is very difficult to know what surgical procedure or surgeon is best for you and what to expect before and after surgery. For these reasons, I feel it’s important to explain the process thoroughly. I have been in practice for over 20 years, have extensive experience, and have taught students and doctors throughout the nation. Given my experience, I feel comfortable sharing my secrets and thoughts with you.
What is a Bunion
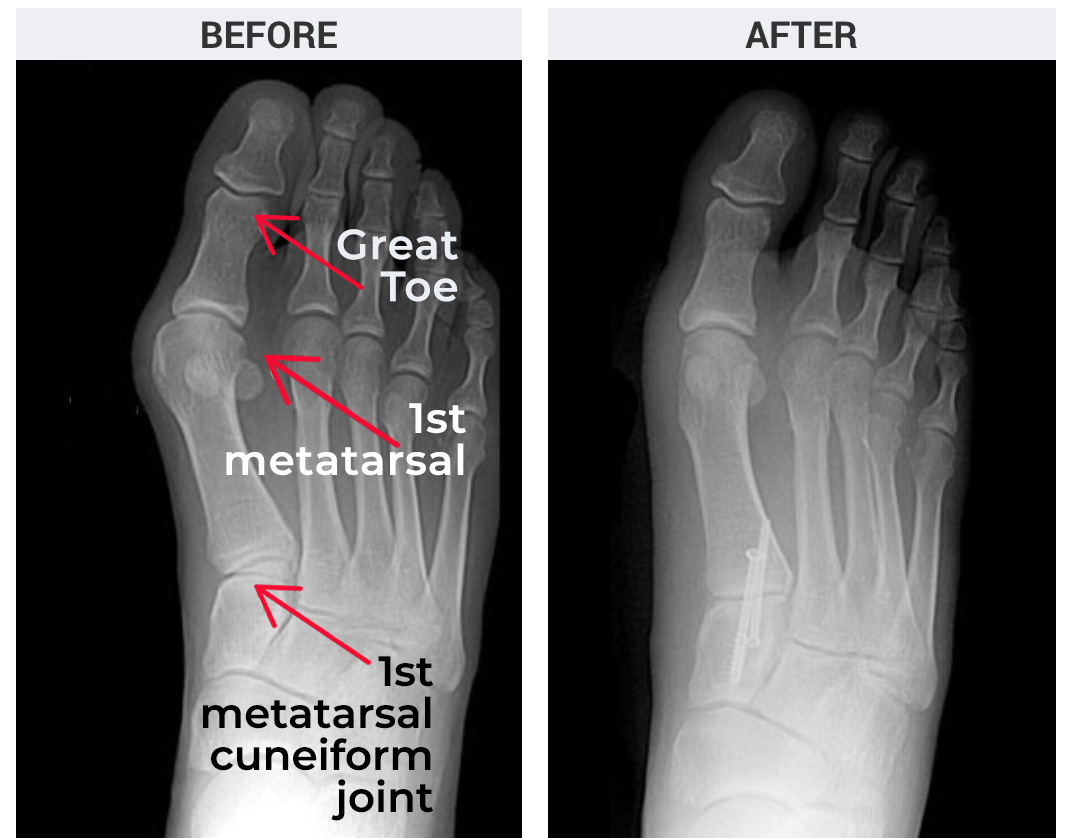
A bunion is a common foot deformity. It is caused by a shift in the first metatarsal–the bone that leads to the great toe. It is NOT an overgrowth of extra bone. As the first metatarsal shifts out, the great toe gets pulled in by a bowing of the tendons. This results in a large bump at the base of the big toe.
Bunions are hereditary, not from bad shoes. While pointy and tight shoes (such as high heels) can add to bunion formation, patients who get bunions have a hereditary laxity of the first metatarsal bone. That laxity is what causes the bunion to form.
When to consider treatment of bunions
The timing for bunion care is very personal and not for a doctor to recommend. You can live with a bunion deformity for life with modification of shoes and activity. Some patients elect to have surgery early in the process while others will wait.
My general insight is that bunions will not get better with time and will only progress. If you have a painful bunion that limits your shoe options and activity, consider fixing the bunion early on. Early surgical intervention is often easier as there is less arthritis, and the deformity is not as complicated to correct. Severe bunions need more invasive surgery, so fixing a bunion early is a smart call!
Are there non-surgical treatments for bunion correction?
Yes! There are several things you can do to limit foot pain caused by a bunion as well as slow down a bunion’s progression. But there is nothing you can do to halt its progression.
The most effective non-surgical bunion treatment is to adequately support the arch of your foot. This is where “custom orthotics” come into the conversation. They are the mainstay of conservative bunion care. Shoes with a wide toe box can also help relieve bunion pain.
Interestingly, most people who have bunions also have flat feet. Due to the flat foot position, there is excess pressure through the first metatarsal bone and big toe joint. The laxity of the bones causes the bunion to form. By supporting the arch with an orthotic or custom insole, the pressure on the big toe joint is reduced.
One thing that will not make a difference is what are called “bunion braces” and “bunion splints.” Braces WILL NOT reduce the bunion deformity or correct the bunion deformity. However, braces and splints can hold the toe in a better position which may reduce some of the inflammation and pain around the bunion.
At our practice, we use a gel toe spacer for some patients to reduce the pressure of the great toe on the second toe, which can help reduce pain. The gel toe spacer can also align the great toe, which can help reduce some of the pain in the great toe joint. Finally, the gel toe spacer fits in shoes well.
If you are looking for conservative care, try an orthotic insole and a gel toe spacer. Easy to use and should be helpful. Remember, you are not fixing anything, and your bunion will get worse with time.
Picking the right doctor is critically important
If you get to the point of considering bunion surgery and are looking for the right doctor, there are a few factors to consider. First of all, should you go with a podiatrist or orthopedic surgeon? The answer is not simple, but here is my opinion: bunion surgery is carpentry. Saw, shift, screw! The material used and techniques used are all carpentry. Bunion surgery does not require a special degree that only one type of doctor has.
What is critically important is that the doctor has good three-dimensional and spatial skills, good surgical hands, is board-certified, and, most importantly, IS NICE to you at all times. Whether things are going great or not so great, your doctor should be nice. These skills are part art and part training.
My personal opinion is to skip the general orthopedist as they are doing knees, shoulders, and other body parts. Stick to foot and ankle surgeons only. They do this work all day, every day, and they are more specialized in their treatments.
Now that you have decided on a podiatrist or orthopedist, how do you pick the right one? Look for someone who educates other doctors and has been involved in surgical training. Usually, doctors who train other doctors have a higher level of skill and are recruited to teach those skills to their counterparts. Also, look at the doctor’s reviews with a fine-toothed comb across multiple platforms.
Remember when reading reviews that billing and money issues are not as much an issue as an actual patient complaint. Patients often complain about bills, payment issues, and insurance company disputes, we’ve all been there. So, look at the reviews, both good and bad, about the reviewer’s surgical outcome, how the doctor treats their patients, how well the office runs, and how easy it was to talk to the doctor and their staff. Remember, all doctors are good until you have an issue and need them. Make sure the doctor is available and easy to get in touch with should you need them.
When you visit the doctor of your choice, make sure the staff is kind and accommodating. Make sure the office is clean, not fancy but clean. Pay attention to how the staff treats you and how comfortable they are treating you for your condition. Do they seem to have protocols set up for your care, or does it feel like the first time they’ve ever seen this problem? You want a doctor and office that feels like a calm and comfortable space, runs like a machine, and takes care of you in a timely and well-planned manner.
Your doctor should X-ray your foot on your first visit. Without an X-ray, it’s hard to get a full picture of the bunion deformity and give proper advice. An X-ray is a must for proper care and advice. Your doctor should review the X-rays with you, educate you on the reason for bunions, how big and problematic your bunion is, and what treatments are best for you.
There is very little need for additional testing before bunion surgery. One new procedure is called a 3-D weight-bearing CT scan. This scan allows better 3-D imaging of the foot and bunion deformity for surgical planning and, although cool, is not always necessary. If a doctor recommends it, I will not say no to it, but it is not essential. In most cases, an MRI or further testing is not really required for bunion planning.
If you are considering surgery, get one or two additional surgical opinions from your doctor. Make sure you educate yourself on the different types of bunion surgeries and understand your options. Get the surgery that is best for you.
My one point of advice is that there are multiple bunion surgeries, and no one surgery is perfect for every patient. Therefore, make sure your surgeon offers various types of bunion surgery.
What bunion surgery option is best for you
Bunions are divided into two types: stable and hypermobile. If the first metatarsal is very lax, a specific type of bunion surgery is required. In the lax cases, the bunion surgery of choice is called a Lapidus bunionectomy. It corrects the bunion deformity by fusing the first metatarsal to the midfoot at its base.
Fusions are usually not ideal in most foot surgeries. But in the case of bunions, the fusion of the first metatarsal at its base is the gold standard procedure. The fusion removes extra laxity in the foot and makes the bone more stable. The joint being fused is a non-essential joint, and there is no true loss of foot function. If you have a very large or very lax bunion, the Lapidus procedure is your go-to.
So why not do the Lapidus procedure for every patient? Well, simply put, the recovery is a bit more difficult. Most doctors will not allow weight on the foot for six weeks (which is the norm). In our practice, there is no weight on the foot for two weeks, and a boot will be worn for six to eight weeks. There is also no way to do both feet simultaneously, and the risk of non-fusion is a bit higher with this type of surgery. Ensure your surgeon does this type of surgery a lot, as it is a bit tougher to do well.
What if you have a small to medium size bunion that is not very lax? Then an osteotomy (or bone cut) is the most common procedure. The metatarsal bone is cut, the head shifted, realigned, and held with pins or screws until the bone is healed.
The osteotomy procedures are subdivided into open osteotomy and minimally invasive osteotomy.
The minimally invasive procedures are great for small to medium bunions and don’t require soft tissue ligament rebalancing. Healing is faster as the soft tissue is opened no more than one to two centimeters, and the joint is left intact. That being said, minimally invasive procedures are a bit more difficult to perform and not perfect for all patients. The doctor needs to be very selective with the right patient for minimally invasive surgery.
The most tried and true bunion procedure is an osteotomy. An incision is made on the top or side of the great toe joint. I personally prefer the side as the incision is more hidden and disappears better. The joint is opened, and the bone is cut and shifted. Most surgeons will use a metal screw to hold the bone. A new technique uses a special fiber pin that holds the bone and then becomes bone by incorporating. This material is truly amazing, and the company, Ossio, is revolutionizing foot and ankle surgery fixation options. After the bone is fixated, the ligaments on the sides of the toes are balanced, and the joint is closed. The surgery takes about 30 minutes and should be like clockwork for most surgeons.
In summary, there are over 40 types of bunion surgeries which are divided into osteotomy and fusion procedures. The correct treatment option depends on the severity of the bunion. If you have a very large bunion or a lax bone, you should consider the Lapidus procedure. If you have a small bunion and not much sideways great toe movement, a minimally invasive osteotomy or an open osteotomy may be best for you. For most patients, an open osteotomy is the mainstay of bunion surgery.
Recovery does and don’ts
During recovery, there are a number of things that you want to keep in mind. For starters, there are three critical factors for good healing:
- Reduce swelling
- Stabilize the foot
- Keep the range of motion in the great toe.
Our regimen is to start patients on anti-inflammatory medication the day before surgery and continue five days after surgery to control swelling. We also use a few special injections during surgery to keep swelling down. We prefer to see patients five days after surgery. A dressing change at this time can relieve some of the tightness and pressure around the foot.
If your doctor wants to see you two weeks after surgery, ask if they can see you earlier. The dressing change is a real comfort factor. We begin home range of motion at five days, moving the toe up and down while controlling the toe’s position.
We officially begin physical therapy at about two weeks post-surgery. This helps reduce swelling and increases range of motion. Some doctors like to use a little surgical shoe after surgery instead of a boot. Although the little shoe is more comfortable, the boot’s security is often preferred in order to protect the bone cut area.
The newest vogue movement with bunion surgery is how quickly you can tell a patient to return to normal shoes. Although it seems cool, you don’t want to be the patient who has a bone that shifts or a screw that breaks because you were put into shoes too early. Please remember that bone healing takes six to eight weeks. With a good osteotomy and solid fixation, return to a stiff sole sneaker is usually okay at four to five weeks but earlier has its risks.
I truly think spending an extra week or two in the boot is a good idea. Don’t risk a bad surgery because your doctor wants to show how great they are. It is not their foot at risk and not a risk worth taking. It’s also important to follow your podiatric surgeon’s instructions to avoid possible complications.
In conclusion, pick your surgeon carefully and follow post-op instructions. Here are some tips:
- Pick a nice surgeon who has a good reputation and will be there for you if there is a problem.
- Pick a kind person. There are many good surgeons but not many who are also good and kind human beings. If you have an issue, the last thing you want is an unkind or inaccessible doctor.
- See two to three doctors before picking the surgeon for you. See if there is an agreement on the type of surgery that is right for you, and always ask the doctor how many types of bunion surgery they perform.
- Remember that minimally invasive bunion surgery, open osteotomy, and Lapidus fusions are the three workhorse procedures for bunion surgery, and good surgeons perform all of them.
- Take care of your foot after surgery and get range of motion exercises started early at home and then in physical therapy. Even if your doctor thinks it’s not needed.
- SLOW DOWN and let your foot heal, especially the first couple of weeks.
- Stay in the boot a bit longer. Some doctors like to show off how early they put you into normal shoes. But you should be more concerned with a great surgical outcome, not how fast you can get into regular shoes.
- Remember, your bone takes six to eight weeks to heal. Don’t rush activity! You can’t beat the body’s real healing properties.
Good luck and cheers to a happy, healthy, and well-aligned foot!