“You can’t love anybody better than a nurse, and nobody will ever love you better!”
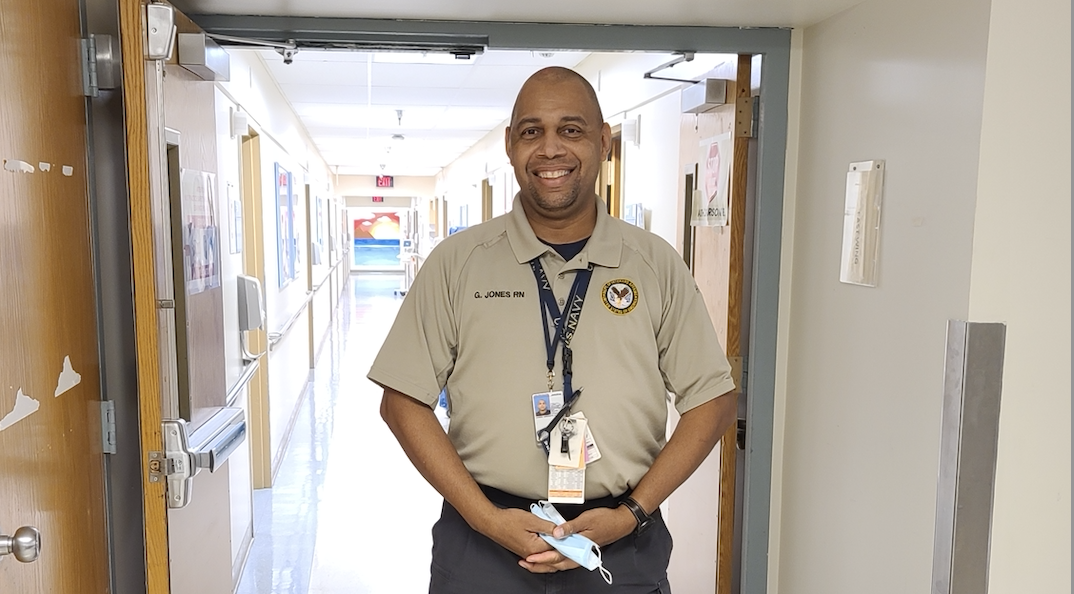
Greg Jones, RN, MSN, CEN (Los Angeles, CA)
Greg Jones is a man who has often traveled the difficult road to beautiful places. He was struggling with nicotine addiction and attending a smoking cessation class when he met a male nurse for the first time. “He was not stereotypical of what I thought a nurse would be and I was like, cool!” Greg had been enlisted in the Navy for 13 years. The nurse told him about a program that would allow him to become a Navy Officer through nursing. Greg had never considered health care. He was a Fire Controlman. His job was to launch Tomahawk missiles off of battleships during the Gulf War. The fight was long and his heart was heavy with the burden of lives lost. He thought this opportunity to become a nurse might be a sign from above. “Nursing was noble. It was a way to balance the lives I had taken. It was atonement.”
Greg’s journey to balance the scales earned him a commission. Soon he was on the other side of the battle, treating wounded sailors as an Emergency Trauma Nurse. The military made sure he was trained in everything from bandages to anesthesia. Now Major Jones was being deployed regularly to hot spots around the globe to save lives. “I was going deeper and deeper into every hot conflict that the U.S. was having.” After 13 more years, Greg sensed he was risking mortality and considered moving his talents to a safer theater: retirement. He thought, “I’m in one piece, so no more jumping out of helicopters for me.”
As Greg was ending his service to the nation, he was also struggling with a divorce. The years of deployment and disconnection had taken its toll on his marriage. He had a beautiful daughter and didn’t want her to suffer from his absence. He was trying to finish his master’s degree in an advanced nursing program and he realized everything was slipping. “Grad school is stressful, and I couldn’t handle it all. I got too many problems. I’m going home.” He left school and moved back to San Diego, California, with his family. The military had one more surprise for him. Greg was sent to Los Angeles to prep an advanced trauma team that was headed to Afghanistan. Coincidently, the First Family was visiting Los Angeles to see the Lakers play the Celtics, and Greg was assigned a medical detail at the Staples Center. He was excited to see the Obamas but didn’t know that the assignment would change his life. That night he met a girl. “I had just got divorced. I thought I’m never getting married [again]. Forget about this. I’m just living my life.” Greg and his second wife have been married five years now and have a two-year-old daughter and a one-year-old son.
He moved to Los Angeles and was hired for a position at the VA hospital. He started as the Assistant Manager of the ER trauma room but was requested to move to the VA Nursing Home because they were struggling for leadership. Greg’s vast experience and training made him the perfect candidate. Things were improving — better structure, better resources, better care for the patients. Then COVID-19 hit. Greg was confident that he could get his staff ready. “I was trained in Ebola, so I’m already used to dealing with communicable deadly diseases. When COVID came to American shores, I rolled out my Ebola practice and planned for the coronavirus.”

Greg’s unit was the first in the VA to segregate COVID positive patients from nonpositive patients. He stopped rotating his staff and retrained them on the proper use of PPE and methods for donning and doffing. He made sure they were comfortable interacting with the patients. “One of the things that happened in nursing, back in the day when we were not wearing gloves and AIDS came along, was these folks wouldn’t be touched. You know, people would just be in isolation. I wanted to make sure that our patients weren’t treated that way this time. At first, we were uncertain about how to manage the spread and treat the coronavirus, so families were excluded from visiting. We had to make sure that we were going in and seeing the patients. That we’re talking to them and holding their hands. It was only those nurses there at their bedside.” Greg’s staff takes pride in working in his unit. “Since this all began in February / March of last year, the members of my staff are still here and they’re still coming to work.” His nurses didn’t leave when they were given the chance to go work somewhere else. “They know we’re taking care of one another as we take care of our nation’s heroes.” As things calmed down, Greg built a visitation window so patients’ families could come and see them and talk through a microphone. Morale improved throughout his facility. It’s all reciprocal. “You can’t love anybody better than a nurse, and nobody will ever love you better!”
While Greg was ensuring the safety of his patients and nurses in the nursing home, he took drastic measures to make sure his family stayed safe as well. His wife had just delivered their son, and their daughter was barely walking. With so little information and no vaccine, Greg decided it was safest to move out of his house. ”I was a stray cat. I lived outside.” He actually moved into an empty house they had been trying to sell. The isolation set in quickly. “I really got into music, trying to learn how to play the guitar.” He learned firsthand what it was like for his patients. “I’m literally standing outside of my living room window at my home, waving at my kids, you know, for an hour.” That was his life from March through May. He was depressed, and he knew it wasn’t good for his patients or his staff. He knew he was being extra safe and testing negative twice a week. He decided he needed to be around his family because it wasn’t good for him mentally to stay away; but he came home with caution. “I would shower and stay in a separate room. But I was still with the family. When I got my negative test, my wife and I could be in the room together with the baby. I was close to people, touching people again, so that just helped.” Greg is relishing every tiny moment with his family. “I’m looking at the small things. You know, I got two little kids. I’m watching my son walk and watching my daughter push him down. That brings me joy.”
Greg is considering every option to help his patients and staff combat this pandemic. He’s looking into animatronics to support patient ease and created a new uniform for his staff to provide them more comfort and protection. Greg knows that the scientists and medical professionals are gaining more knowledge each day, but he feels that it’s the work of the nurses that is changing the tide on the pandemic. “I link it back to the African griots, you know, the oral tradition of sharing. Look, this is what works for this. It didn’t work. Okay. Hey, you know what? I found this. Let’s try.” Small things like resting a patient on their side instead of their back for better breathing, or turning their bed so they look out the window to the left instead of the right are helping patients survive. He also recommends everyone gets vaccinated. He considers the vaccine another weapon in this battle against COVID-19. “Should I contract it, I’m more than likely not going to die. I want every piece of armor and every weapon I can have. Why not take another piece of protection?”
#FirstRespondersFirst Microstep
When you’re feeling stressed, remind yourself why you became a healthcare worker in the first place.
If you joined this field because you want to help people, remembering that fact can help you to move through challenging moments with more resilience.
Greg’s story is part of “Unmasked: Profiles of Humanity and Resiliency,” a collection of stories from the frontlines published by the National Black Nurses Association (NBNA) in partnership with #FirstRespondersFirst. The NBNA offers therapy and wellness services through RE:SET, a free mental wellness program developed for Black nurses to help them RE:SET, recharge and widen their circle of support. Visit nbnareset.com to learn more.