Hospital based clinicians are highly mobile throughout the day. Direct and indirect patient care requires dependence on mobile devices and the frequent need to work across different units or floors to complete documentation, communicate with colleagues, review charts, respond to patient portal messages, and complete required compliance training modules – all of which are often time sensitive and require access to dedicated space for focused work.
The clinical workspace must accommodate diverse task demands and complexity, allowing for collaboration while maintaining confidentiality; accommodating team dynamics without disrupting individual focus. Spaces also need to be comfortable or at very least do no harm, as clinicians are subject to long shifts and work at all hours.
The Challenge
There is growing attention to the impact suboptimal work environments have on healthcare providers. Factors like lack of natural light, stagnant indoor air quality, near constant alarms or signals (to the point of alarm fatigue), varied thermal conditions, limited privacy and frequent interruptions take a physical and mental toll. Prolonged exposure to these physical, environmental and psychological factors jeopardizes clinician health and performance.
Given the challenges caused by space constraints in most urban hospitals and the prioritization given to patient spaces, ergonomic human centered design of clinician workspaces is unfortunately not always the norm – making it necessary to provide clinicians with portable ergonomic tools and training to create an ergonomic setup wherever and whenever possible. Furthermore, it’s important to examine systemic opportunities to enhance physical and mental well being through access to beneficial, effective resources.
Ergonomics Solutions & Strategies
Ergonomics is an important element of the broader systemic effort to enhance wellness in the clinical workspace. With emphasis on physical, environmental, cognitive and organizational forces, ergonomic intervention seeks to create systems and standards that help clinicians do their best work without sacrificing their personal health.
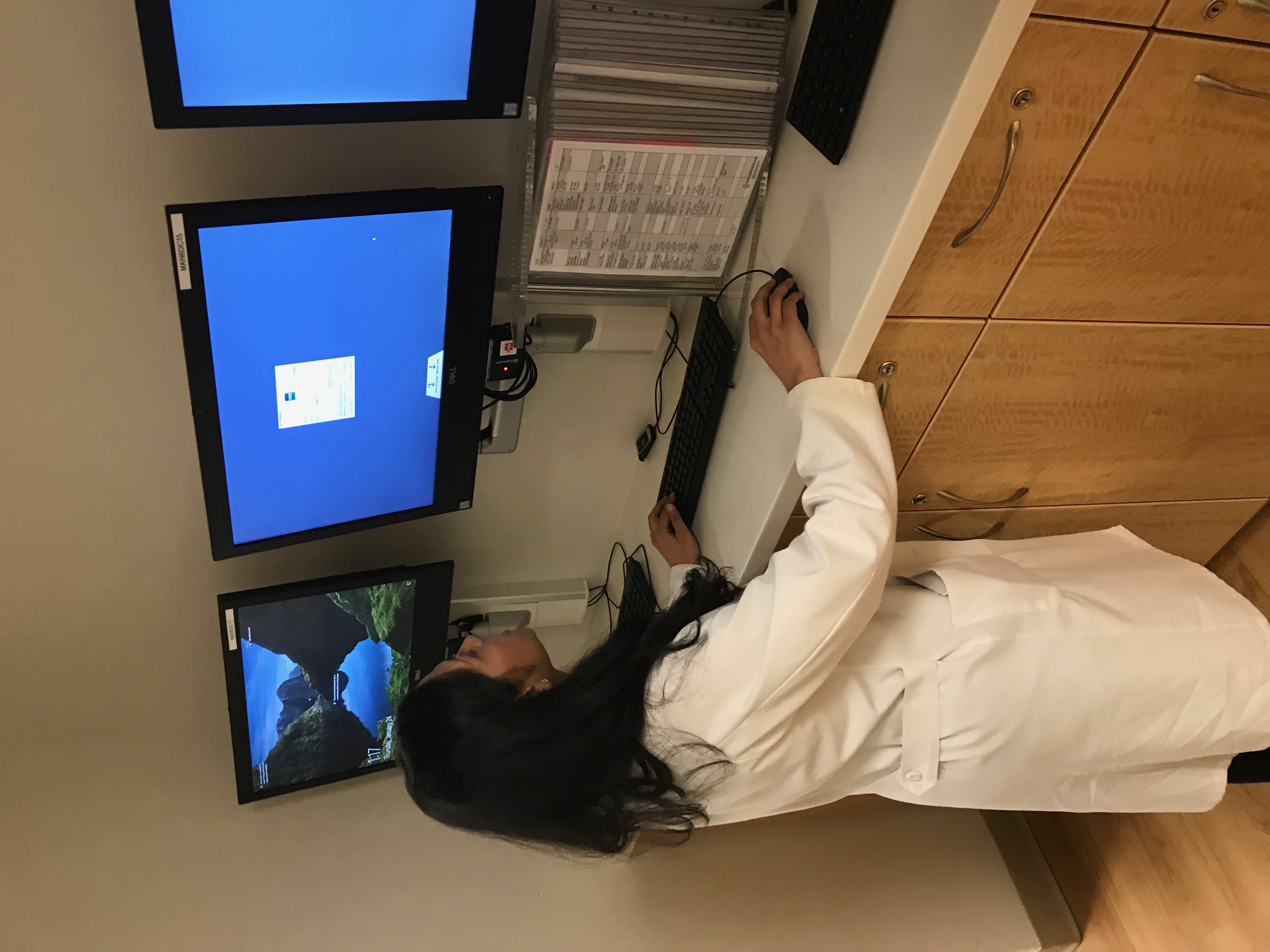
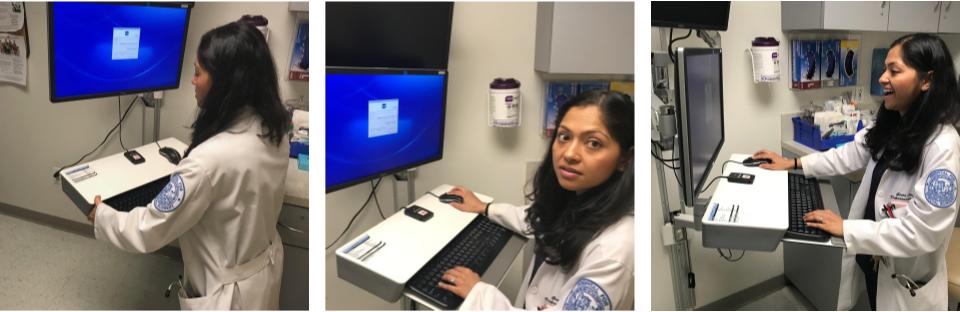
Starting with the physical environment, every clinical workstation should include standard ergonomic equipment including supportive seating, and adjustable peripherals. Specifically, a chair with adjustable seat height and depth, multi-axial armrests and lumbar support, or active seating solutions that allow the clinician to briefly rest in a supported position as an alternative to static standing for prolonged periods. Peripherals like the keyboard and mouse should be positioned on a surface that is within a comfortable range for the user (or can be adjusted) without requiring excessive reach to access, and screens (monitors, tablets, etc) should ideally be mounted on a flexible arm to allow adjustable height, depth and rotation to promote neutral head and neck posture to view.
Of equal importance is understanding the ‘anatomical landmarks’ to make necessary adjustments that help clinicians quickly adapt a workspace to their body in any situation. It takes a bit of time and training to develop a feel for the optimal setup based on individual stature and functional demands, but the benefits are significant.
The best analogy we give clients is to think about what happens when you get into the driver’s seat of a car you’ve never driven before. Instinctively and almost subconsciously, you begin making adjustments to enhance comfort, safety and performance: You immediately adjust mirrors to ensure necessary visibility, you fiddle with the steering wheel height and angle so that you can reach it comfortably, you quickly size up the adjustability features of your seat – moving the seat forward or backward depending on your height, straightening or reclining the seat back, increasing or decreasing the degree of lumbar support, adjusting the headrest angle, and even specifying the temperature of the heated seat. You also set up access to resources like navigation and traffic alerts to eliminate cognitive stresses when making quick decisions on the road, and music or podcasts in order to make the journey ahead an enjoyable experience.
Yet when sitting down at a new workspace, most people seldom make any of the necessary adjustments for improved comfort or efficiency. Plus, clinicians don’t always have habits or strategies in place to introduce efficient rest breaks, stretches or movement or into their workday. Applying the same rationale to the workspace requires the training, reinforcement and a bit of practice over time to eventually develop the skills and body awareness to adapt the work environment for comfort, safety and performance.
Equipped with an understanding of how the work setup should accommodate stature, the next challenge is enforcing behavioral change in the form of breaks at regular intervals. While scheduled breaks are likely not always feasible, a simple visual cue such as wall signage in a common area or monitor screen savers promoting micro-breaks are helpful, low cost measures to elicit a quick postural adjustment or stretch. A variety of mobile and desktop apps also prove effective in providing a gentle nudge to implement rest breaks throughout the day. Maybe a cue as simple as seeing a colleague take a moment to stretch could trigger a contagious response in others!
A Culture of Support
Perhaps the biggest and most important hurdle is gaining collective support amongst clinicians in favor of systemic change. Traditionally embedded practices don’t always align with current workplace wellness trends, as clinicians face challenges to their physical and mental endurance despite evidence linking such work conditions to burnout. A culture shift prioritizing self care and wellness has been increasingly embraced by the new generation of upcoming clinicians that are witnessing the repercussions of neglect. Building healthy work practices into clinician training, workflow and culture requires ongoing observation and study of how clinical teams support each other, and are supported by the healthcare system to champion self care initiatives.
Progress is evident with the increasing presence of the Chief Wellness Officer role – an acknowledgement that wellness needs organizational advocacy, prioritization, reinforcement and leadership representation for lasting impact and better future outcomes for all.
#worksmarter #workplacewellness #ergonomics #employeeexperience
References:
1 Sen, S., MD, PhD. (2019). It’s time to get serious about resident wellness. Association of American Medical Colleges. Retrieved from: https://news.aamc.org/medical-education/article/its-time-get-serious-about-resident-wellness/
2 Healthcare Design: “Reworking the Healthcare Workspace” (2014). Retrieved from: https://www.aafp.org/fpm/2013/0300/p20.htmlhttps://www.healthcaredesignmagazine.com/trends/operations-facility-management/reworking-healthcare-workspace/
3 Applied Nursing Research:Nurses’ perceptions of how physical environment affects medication errors in acute care settings” (August 2009). Retrieved from: https://www.sciencedirect.com/science/article/pii/S0897189709000810
4 Health Facilities Management:”How a risk management focus can improve the physical environment” (April, 2018). Retrieved from: https://www.hfmmagazine.com/articles/3313-how-a-risk-management-focus-can-improve-the-physical-environment
5 Kirch, D (August, 2017). Building a framework for clinician well-being and resilience. Association of American Medical Colleges. Retrieved from: https://www.aamc.org/news-insights/building-framework-clinician-well-being-and-resilience
6 American Association for Physician Leadership. “Chief Wellness Officer: New Opportunity, Necessary Role” (2019). Retrieved from: https://www.physicianleaders.org/news/chief-wellness-officer-necessary


