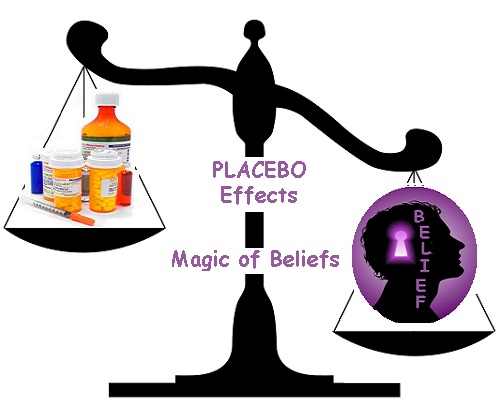
Is the placebo effect real?
A placebo is a medical treatment or procedure designed to deceive the participant of a clinical experiment. It does not contain any active ingredients but often still produces a physical effect on the individual.
Placebos are essential to the design of reliable clinical trials. Their once-surprising effect on participants has become the focus of many studies.
The placebo effect refers to the impact of a placebo on an individual. Even inactive treatment has repeatedly demonstrated a measurable, positive health response. The power of the placebo effect is considered to be a psychological phenomenon.
Fast facts on placebos
The placebo effect has been measured in thousands of medical experiments, and many doctors admit to regularly prescribing placebos.
Drug companies must show that their new drugs work better than a placebo before the drugs are approved.
Placebos have been shown to affect a range of health conditions.
The colour of a tablet can alter the strength of its placebo effect, and larger pills induce a stronger effect than smaller pills.
Some believe the self-healing properties of the placebo effect can be explained by evolutionary biology.
Placebo medications contain no active ingredients but if the participant thinks they are taking medicines, a placebo can improve their physical condition.
The placebo effect describes any psychological or physical effect that a placebo treatment has on an individual.
The placebo has become an essential part of all good clinical trials.
In early clinical trials, the capabilities of a new drug were measured against a group of people who took no medication. However, since discovering that the simple act of taking an empty tablet can produce the placebo effect, it is now considered essential to have a third group of participants.
This additional group takes a tablet containing no active ingredient to measure the response against them. Participants in this group will take a sugar pill, for example.
A drug is only approved when it produces a greater effect than a placebo.
Placebos have been shown to produce measurable, physiological changes, such as an increase in heart rate or blood pressure. However, illnesses that rely on the self-reporting of symptoms for measurement are most strongly influenced by placebos, such as depression, anxiety, irritable bowel syndrome (IBS), and chronic pain.
Placebo interventions vary in strength depending on many factors. For instance, an injection causes a stronger placebo effect than a tablet. Two tablets work better than one, capsules are stronger than tablets, and larger pills produce greater reactions.
The placebo effect changes from individual to individual, and its strength varies from one disease to the next. The reasons for the influence of a placebo are not fully understood. Given the variation in response, it is likely that there is more than one mechanism at work.
Below are four of the factors said to be involved in the placebo effect.
1. Expectation and conditioning
Part of the power of the placebo lies in the expectations of the individual taking them. These expectations can relate to the treatment, the substance, or the prescribing doctor.
This expectation may cause a drop in stress hormones or cause them to recategorize their symptoms. For instance, a “sharp pain” might instead be perceived as an “uncomfortable tingling.”
On the other hand, if the individual does not expect the drug to work, or expects there to be side effects, the placebo can generate negative outcomes. In these cases, the placebo is instead referred to as a nocebo.
Placebo opioids to participants who had recently taken genuine opioids. A well-documented side effect of opioids is respiratory depression. The researchers found that the placebo drug elicited respiratory depression, despite having no active ingredients.
Some believe that classical conditioning might play a part in the placebo effect. People are used to taking medication and feeling better. The act of taking a drug elicits a positive response.
Conditioning and expectation are separate mechanisms, but they are likely to be related.
2. The placebo effect and the brain
Brain imaging studies have found measurable changes in the neural activity of people experiencing placebo analgesia. Areas that have been implicated include parts of the brain stem, spinal cord, nucleus accumbens, and amygdala.
Strong placebo responses have also been linked to increases in dopamine and opioid receptor activity. Both of these chemicals are involved in reward and motivation pathways in the brain. Conversely, nocebos have been found to reduce dopamine and opioid receptor activity.
Some of these neurological changes occur in areas of the brain that are often targeted by antidepressant drugs. This might account for the 50 to 75 percent placebo response rate in antidepressant trials.
3. Psychoneuroimmunology
Psychoneuroimmunology is a relatively new area of scientific study. It studies the direct effect of brain activity on the immune system. Just as a dog can be conditioned to salivate at the sound of a bell, so can mice be conditioned to restrain their immune system when presented with a specific stimulus.
It has long been known that a positive outlook can help stave off illness. In recent years, this pseudo-science has become science fact. Expecting improvements in health can impact the efficacy of an individual’s immune system.
The pathways by which the brain does impact the immune system are complex. An explanation has only recently started to form. There is a possibility that this type of interaction plays a role in the placebo effect.
4. Evolved health regulation
One explanation for the placebo effect is the evolution of a human brain’s ability to moderate healing.
The body of a mammal has developed helpful physiological responses to pathogens.
For instance, fever helps remove bacteria and viruses by raising the internal temperature. However, as these responses come at a cost, the brain decides when it will carry out a certain response.
For instance, in late pregnancy or during states of malnutrition, the body does not carry out the fever response to infection. A raised temperature could harm a baby or use up more energy than a starving individual can spare.
The evolved health regulation theory suggests that a strong belief in a medication or intervention might relieve symptoms. The brain “decides” it does not need to mount the appropriate response, such as fever or pain.