This is a re-blog; originally posted just over one year ago; despite this, it keeps coming back to me. Recurring like a nightmare. People manipulated into the helplessness of patients, sent down one-size-fits-all avenues and, with the recent winter, more and more pressure to standardise, streamline, create flow.
I am convinced that although pathways do help in many situations, improving quality and likely patient safety, they are also a significant hazard to those people who don’t fit-in; mostly, you and me.
x x x
Pathways are everywhere in medicine. In fact, I don’t believe you can move anywhere – into hospital or out, from A to B or doctor Y to Z without being caught-up in some sort of clinical, hierarchical or organisational pathway.
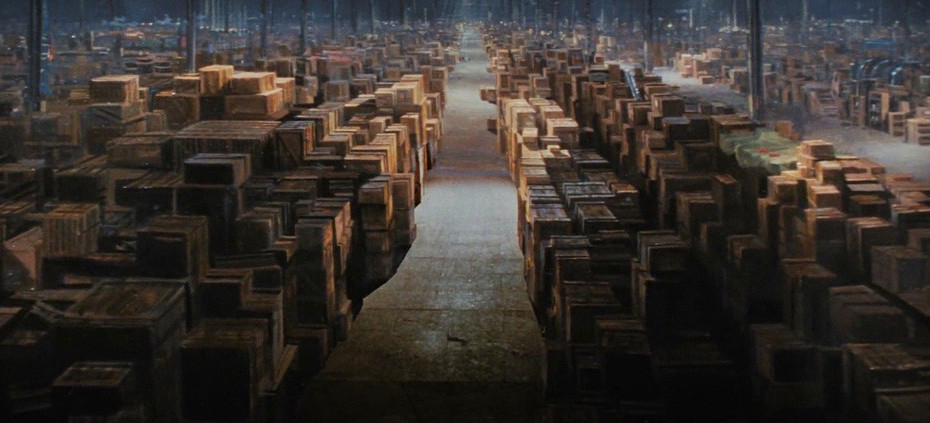
There is an expectation that patients – that is, people, will follow pre-planned, coordinated and arranged routes. A little like the movement of sausages or boxes or motorcars in a factory.
People, oddly, aren’t like boxes. For although boxes do come in all different shapes and sized, colours, textures and designs, they aren’t quite as complicated – they don’t feel fear or pain, aren’t conscious, and even if they were, they would likely not perceive the world in a similar way to people – to a box, the world is the world, is the world.
None of my patients seem to fit-into pathways, and that is a problem, for, as I say, the system is bedevilled with them. Pathways, in some instances are great – they let those in charge know what is happening – or, should be happening, at any moment in time, they are part of the process for reducing variability – an enemy of quality, and, they allow planning, prediction and forecasting.
People just don’t necessarily coincide with these pathways, particularly in medical – as opposed to surgical, disciplines, where variation is seen as a virtue in the former, a complication in the latter.
Again, it is odd, perhaps no coincidence, that the area of medicine that interests me most – delirium, derived from the Latin, ‘to deviate from the furrow’ is in effect a translation of this difficulty. None of my patients keep to the furrow, and that is what I love – the complexity of people, with their infinite variety, combined with the ever-changing presentation of disease and illness;
This is also part of how we, my colleagues on the ward work with our patients – that is, having a broad interpretation of what is OK, what is right, when to get-up, how much to eat, how to walk, what clothes to wear, how to say hello.
A fundamental of dementia care is appreciating that the reality you perceive is very possibly different to that of your patient. Trying to bend their will, distort their vision so that it is closer to yours, does not work. You need to move your understanding, your reality into that of the other.
The neat pathway you have constructed, spent many hours fiddling-with on the computer, just won’t work – you need to move the pathway to where the person is standing, adjust the light to what they need, taper the medicines, adapt.
Let us move the paths to fit the needs of our patients, let us re-format the routes to recovery, to treatment and care, let us not manipulate the patient or the data, let’s change our responses or behaviours, to fit what is needed.
Perhaps, the next time you find yourself, your mum, dad, or friend the victim – subject of a clinical pathway that doesn’t entirely fit with their apparent needs, call-out; ask the doctor or nurse to explain why, ask for clarification – the process should at the very least be logical. Don’t accept platitudes.
Patients first!

Originally published at almondemotion.com