When Dr. Richard Benson gets a text message that reads “Code 1,” he knows he’s needed at MedStar Washington Hospital Center in Washington, D.C., to treat someone who’s suffered an acute stroke.
He also knows the patient is probably between 40 and 60 years old and has other serious health issues.
When Benson gets a text message on his other pager that reads “Code Stroke,” he knows he’s needed at Suburban Hospital in Bethesda, Maryland, to treat someone who’s suffered an acute stroke.
He also knows the patient is probably between 70 and 90 years old and facing other age-related issues.
The challenges are similar but different. They’re a byproduct of many things, including affluence and education level, both of which are higher in the suburban location.
“Different hospitals, different patient populations,” Benson said. “You do have to look at them differently. It helps to know what to expect.”
Benson, of course, makes no distinction between patients or hospitals. A stroke is a stroke, and he’s devoted his career to treating them.

The reason he mentions the difference is to underscore his key message: The best way to beat a stroke is to keep it from ever happening. And the best way to do that is to know your risks and do something about them.
So as May winds down, and the spotlight of American Stroke Month fades, Benson and the entire stroke community want conversations to continue about preventing this cruel disease – the No. 5 killer of Americans and a leading cause of long-term disability among adults.
If you remember only one stat about stroke, let it be this: 80 percent are preventable.
Again:
4 of every 5 strokes could’ve been prevented.
“There are risk factors we define as ‘modifiable’ and ‘non-modifiable,’” Benson said. “Non-modifiable risks factors are things you can’t do anything about: age, race, gender, family history. The modifiable risk factors are things we can do something about.”
Controlling high blood pressure, also known as hypertension, tops the list.
Getting BP within normal ranges has long been a reliable way to reduce all sorts of medical risks. This became even more important – and more of a challenge – in November, when new guidelines released by my organization, the American Heart Association, adjusted the scale of what’s considered a safe number.
High blood pressure is now classified as a reading of 130 on top or 80 on bottom. The standard had been 140/90. As a result, the ratio of Americans with HBP went from nearly one in three to nearly one in two.
“This change will hopefully get providers talking more about modification techniques and getting numbers under control,” Benson said. “Just by controlling blood pressure, getting it down, we could significantly decrease the number of strokes as well as the number of stroke deaths.”

Controlling blood pressure doesn’t necessarily mean taking a pill. In many cases, it’s as simple as making lifestyle changes, the same ones that help ward off many other threats to your heart, brain and body.
“Make sure you are exercising for 20 to 30 minutes at least three days a week, more if possible,” Benson said. “Try to follow a Mediterranean diet – eat more fruits, vegetables, fish, olive oil and nuts. Don’t smoke. If you drink, don’t have more than two glasses per day for men and one per day for women. Obviously if you have diabetes, it’s important to keep blood glucose under control. If you have high cholesterol, you may benefit from taking statins.”
Clearly, there’s plenty to modify.
While your healthcare professional can guide you through some of those risks, you probably already have an idea about some other changes to make.
You also already know some of your non-modifiable risk factors.
African-Americans are twice as likely as white people to have strokes. Hispanics are 1.5 times as likely as white people.
Starting at age 65, the risk for stroke increased about 1 percent each subsequent year.
“Another interesting thing is socioeconomic status: The lower the status, the higher the risk,” said Benson, pointing to the wide difference in the type of patients he sees at those two hospitals that are about 10 miles apart.
After prevention, another major effort is spreading awareness. That is, would you know if someone is having a stroke?

Remember the acronym FAST. If you see Face drooping, Arm weakness or Speech difficulty, it’s Time to call 911.
“Some people don’t call an ambulance because they think it’ll go away or they don’t want to notify their neighbors,” Benson said. “However, time is brain. The longer you wait, more cells can potentially die.”
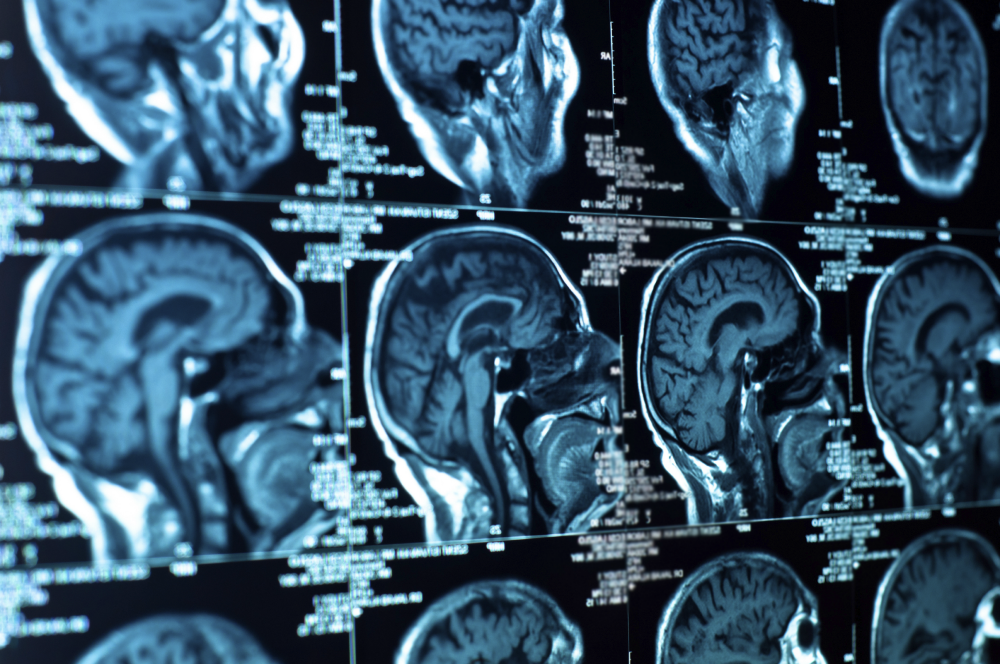
Benson is associate medical director of the Comprehensive Stroke Center at MedStar Washington Hospital Center. Along with Suburban hospital, his work is connected to research for the National Institutes of Health. It involves possible stroke patients getting an MRI as a first step to help diagnose their problem and map out a treatment plan.
Early results have been promising. A pilot program could follow. In years to come, this could turn out to be standard protocol.
And, hopefully, by then fewer people will be suffering strokes.