
The research body of evidence linking the major role of the exposome as a whole and toxicants in particular to chronic disease continues to grow. Data from Covid-19 deaths show that the contributions of chemical body burden to how severely the symptoms from this disease manifest in each individual cannot be overlooked.
The exposome as a concept has been defined for more than ten years. The exposome consists of environmental pollutants, dietary constituents, psychosocial stressors, our microbiota, and physical factors such as infections and Single Nucleotide Polymorphisms, which work upon the genome, which is fixed, to produce certain gene expressions, which are fluid. This is a new field called epigenetics, which has transcended the “genes as destiny” dogma and expanded our understanding of what contributes to disease and what contributes to health.
As the data from China and Italy demonstrate, 99% of the mortality is derived from individuals with one or more chronic diseases.
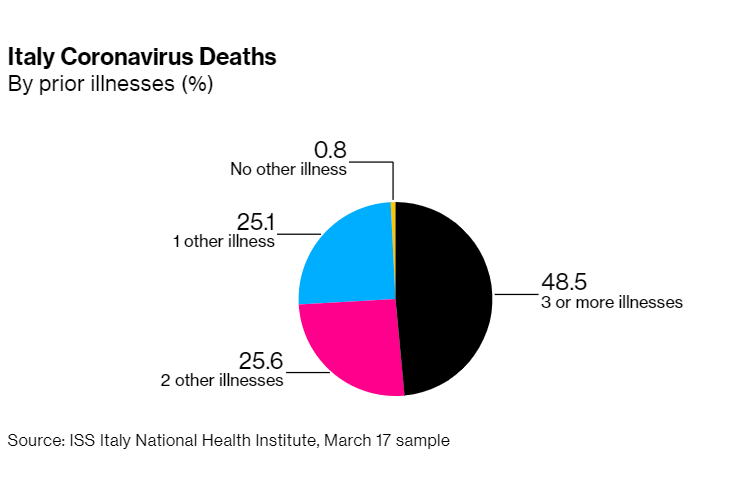
These chronic illnesses include obesity, diabetes, liver, kidney and cardiovascular disease, as well as diseases that affect the lungs including asthma, allergy, emphysema, and chronic obstructive pulmonary disease (COPD).
Most Americans are suffering from one or more of these chronic diseases that the Centers for Disease Control (CDC) have identified as increasing the risk of death from Covid-19. The prevalence of these conditions has risen parallel to the breathtaking rise in harmful chemicals over the past few decades, from plastics, agricultural chemicals, flame retardants, perfluorinated compounds found in water repellent and stain resistant items, heavy metals, and polychlorinated biphenyls (PCBs), which has been banned since the 1970’s, all of which incidentally have been found in the cord blood of newborn babies. Even our babies are being born pre-polluted.
These underlying chronic diseases illuminate the role than an already-weakened immune system plays in becoming susceptible to any infection, and highlights that our immune status and health are key indicators in morbidity and mortality. This is an important take-away from the current pandemic situation, and the basis for taking action now to preventatively create optimal health.
A troubling insight into global health dysfunction is a growing body of evidence that we are slowly poisoning ourselves with the very same products that were designed to make our lives easier and certainly more convenient. Think plastics.
Research is now supporting that toxicity, as part of the exposome, is the main driver of disease. Indeed the determinants of health are not so much your genes, but your total body burden or load of toxicants, how well you can eliminate or detoxify them, and your own matrix of Single Nucleotide Polymorphisms (SNPS) which are variations in your genes that impact your liver’s ability to detoxify xenobiotics from one person to the next, among other things.
This brings us to the Elephant in the Room:
“We are an unhealthy nation—and many of our elevated disease rates are linked to environmental chemicals. COVID-19 is bringing into sharp focus the need to prevent this widespread exposure.”
Linda S. Birnbaum and Jerrold J. Heindel
The CDC has been tracking toxicants in our blood for decades. The updated CDC National Report on Human Exposure to Environmental Chemicals (www.cdc.gov.exposurereport) has now measured 242 toxic chemical and metal pollutants in the blood and urine of U.S. residents. Half of those- 120 of the toxic compounds- were found in 100% of the participants! We have released over 85,000 new chemicals into the environment in the last 80 years, of which only 242 are tested for. It makes you wonder how many chemicals we really have inside of us. Some research labs have done expanded testing and found 20-30,000 chemicals in the blood of those tested.
These chemicals have already demonstrated immunotoxicity and damage to mitochondria (energy factories in our cells) in the published literature. All are potent pro-oxidants and deplete glutathione, our body’s top detoxifying enzyme and endogenous anti-oxidant. These ubiquitous toxicants have demonstrated not only immunotoxicity, including autoimmunity (a global epidemic), but neurotoxicity (rising rates of Alzheimer’s and Parkinsons) and endocrine toxicity (they mess up your hormones).
This means there is an inverse correlation between toxins and immune function – meaning toxins dysregulate the immune system making it less vigilant against invaders and more likely to create negative immune reactions. Toxic load must be addressed in order to achieve optimal immune function.
Let’s look at the top two chronic diseases, obesity and diabetes, that seem to predispose to an unfavorable outcome to infection with SARS-Cov-2, and the chemical pollutants that strongly contribute to them.
Since 85 percent of diabetics are overweight or obese, and 30 percent of overweight/obese people have type 2 diabetes, these two underlying conditions alone interact to make Americans particularly susceptible to Covid-19 and its complications.
Obesity
According to a paper in pre-review entitled “Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City” doctors at NYU Langone Health center conducted the largest study so far of US hospital admissions for COVID-19. They found obesity was the biggest deciding factor in hospital admissions, which may suggest the role of hyper-inflammatory reactions that we see with the disease.
“The chronic condition with the strongest association with critical illness was obesity, with a substantially higher odds ratio than any cardiovascular or pulmonary disease,” writes lead author Christopher M. Petrilli of the NYU Grossman School.
Obesity, defined as a BMI over 30, has been rising along with the overall chemical production in this country. The commonly held causes of obesity-overeating and inactivity-do not explain the current obesity epidemic.
Obesogens
The term obesogen is now applied to certain Endocrine Disrupting Chemicals (EDCs) that cause weight gain. EDCs are used to describe chemicals that act like hormones on the body, and in extremely tiny doses just like our own hormones. Two classes of the biggest obesogens that are ubiquitous in our environment are bisphenols and phthalates, found commonly in many of the consumer products that we use and are exposed to every single day.
Bisphenols
The bisphenol family contains bisphenol A, which due to widespread concern about its negative health impacts has also been partially replaced by bisphenols S, F, and AF, which unfortunately have about the same problems as the chemical compound they are replacing.
The bisphenols family, consisting of BPA, BPF, BPAF and BPS, is present in 95% of Americans according to NHANES data from 2013-2014. Specifically, BPA was found in 95.7%, BPS in 89.4%, and BPF in 66.5% of U.S. participants.
Bisphenols are high-volume industrial chemicals found in products containing polycarbonates (food and water containers) and epoxy resins such as found in canned goods. Over 5 million tons are produced globally annually. They are commonly found in canned foods, thermal receipts, and food contact materials, but they will never be listed on the label.
Currently many products are available that will claim on their label that they are BPA-free, but this may mean that a regrettable substitution such as BPS may have been used instead, which leads to roughly the same health complaints.
Bisphenol A and its metabolites cross the placenta and have been found in amniotic fluid, fetal tissue, and cord blood. Fetuses and newborns have a limited ability to metabolize BPA and instances of negative pre- and post-natal effects associated with elevated BPA levels have been found.
Fetal exposures to BPA at levels equivalent to, or below the established daily human safe-dose (50µg BPA/kg body weight/day) not only increase body weight and postnatal growth rate, but also alter body composition in later life.
In adults participating in the 2003-2006 NHANES trial, those with urinary BPA in the second quartile and above, had increased rates of obesity. This means that a full 75% of the adults measured in that time frame had an increased rate of obesity, with the adults in the second quartile having an 85% greater risk!
In a recent meta-analysis published in 2020, BPA was found in all urine samples collected from both sexes and found to be significantly associated with obesity.
Phthalates
The phthalates chemical family also has also been found to promote obesity.
These are never listed on the label and so you need to know where they hide. Phthalates are comprised of a family of low molecular weight phthalates used primarily in fragrances and nail polish, and a family of high molecular weight phthalates used in plastics. 95% of Diethyl-hexyl phthalate (DEHP) is used in polyvinyl chloride (PVC). DEHP makes up 30% of PVC which can be found in plastics, flooring, shower curtains, adhesives, raincoats, hoses, IV tubing, and toys. Phthalates are not closely bound to the underlying material and migrate into the air and leach into whatever they touch. They are absorbed through skin from personal care products that contain them, and also through ambient air.
The low molecular weight phthalate diethyl phthalate (DEP) is found in 71% of cosmetics tested and 100% of fragrances tested.
The low molecular weight phthalate dibutyl phthalate (DBP) is found in 67% of nail polish.
Phthalates are present in indoor dust samples, blood, urine, breast milk, sweat, and cord blood of infants.
Phthalates are found in plastics, food contact materials, and personal care products, and are ubiquitously found in the blood and urine of U.S. individuals.
Phthalates levels in both adult males and females have been positively associated with waist circumference and truncal fat mass.
In a recently published study of post-menopausal women, the women in the highest quartile of measured urinary phthalates were two times more likely to be overweight and three times more likely to obese, compared to those in the lowest quartile.
Diabetes
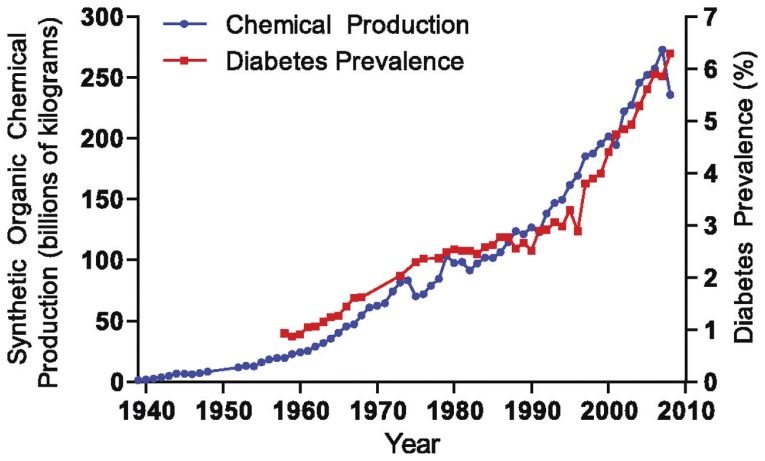
The U.S. leads developed nations in type 2 diabetes incidence. Currently 11% of Americans have type 2 diabetes, compared with 0.9% in 1958, a 10-fold factor increase in about 50 years.
The graphic below from the Journal of Diabetes and Its Complications (2007;21(6):363-370) correlates the rise in diabetes with the rise in Persistent Organic Pollutants (POPs). Individuals in the top quintile of exposure to six common POPS had a dramatic 37.7 fold increased risk for type two diabetes. Eating too many calories and not exercising enough is no longer adequate to explain the rising rates of diabetes in the U.S.
Bisphenols
While epidemiological research has indicated a positive association with BPA and diabetes, a longitudinal study published last year looked at serial measurements of BPA and BPS over 9 years and the risk of developing type 2 diabetes and found that compared with participants with the lowest average BPA exposure (below the first quartile), participants in the second, third, and fourth quartile groups of exposure had a near doubling of the risk of type 2 diabetes.
Phthalates
Phthalates are endocrine disruptors. In animal models, they have been shown to interfere with adipocyte biology (that is, fat cells) and glucose (sugar) metabolism by their effects on the peroxisome proliferator- activated receptors called PPAR receptors.
In human studies, DEHP has been found in young nurses in the Nurses Health Study II. Younger nurses with higher levels of urine phthalates were found to have twice the incidence of type II diabetes than those with the lowest levels.
In a meta-analysis of all studies prior to 2014, the difference in risk for type II diabetes between those with the highest levels of urinary phthalates and the lowest was statistically significant- people with higher levels of phthalates excreted in urine were 1.5x more likely to have type II diabetes.
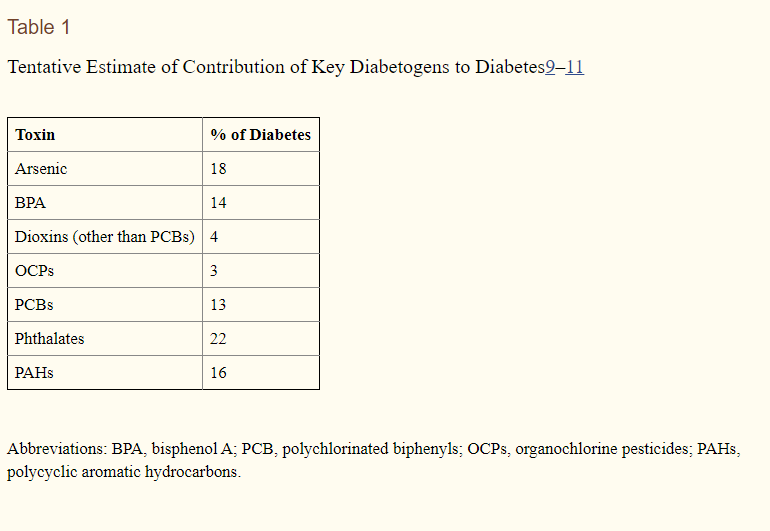
In Table 1 above, the tentative estimate of contribution of key diabetogens, which are defined as chemicals that kills pancreatic β-cells or disrupts their function, to diabetes is listed.
Just the two toxins discussed in this article, BPA and phthalates, total 36% of the tentative chemical contributions to diabetes. This suggests that gaining control over exposures to these two chemicals would result in a lower risk of developing type II diabetes.
“The current conundrum regarding toxicant exposure and diabetes must be directly addressed and a proposal for immediate action must be created, consensus reached and communicated to all healthcare providers. Legislation to eliminate bisphenols and phthalates from commerce is eventually unavoidable. Green chemistry has already provided plant-based plastics that do not have endocrine disruptor properties, which will not be just another regrettable substitution.”
–Lyn Patrick, ND
Conclusion
We need to expand our investigation and understanding of what impacts our immune system in order to successfully navigate this and future pandemics. Starting with a lower body burden of harmful chemicals will turbocharge your immune system and reduce your risk of pre-existing conditions, giving you a better quality of life now and a better chance of fighting off seasonal diseases, other infections, the Sars nCoV-2 virus, and other nasty pathogens which may emerge in the future. Doctors and researchers around the world are in a race for a cure or vaccine for the Sars nCoV-2 virus now that it is widespread, especially in people with weakened immune systems who are older or have pre-existing conditions. The Western insurance model of medicine focuses on resolving illnesses or injuries caused by a specific agent, or masking symptoms of chronic lifestyle diseases with many contributing factors (e.g. Type II diabetes), typically with the use of medication. A healthier population in general would not have reduced the contagiousness of this disease, but would likely have reduced its mortality and devastating impact to families, society, and the economy. A paradigm shift to supporting total wellness of the body by reducing exposure to environmental toxins in our food, water, cosmetics, packaging products, and everyday life, in addition to education about healthy lifestyle choices and making those lifestyle choices accessible for everyone, is a wise investment in future health for everyone in society.
References:
Ebhardt T, Remondini C, Betraccle M, 99% of Those Who Died from Virus Had Other Illness, Italy says. Bloomberg, 3/18/20
https://www.ewg.org/research/body-burden-pollution-newborns accessed 4/19/20
https://www.ehn.org/chemical-exposure-coronavirus-2645785581.html accessed 4/19/20
Crinnion W, Pizzorno J. (2019). Clinical Environmental Medicine: Identification and Natural Treatment of Disease Caused by Common Pollutants. St. Louis, Missouri. Elsevier.
Baille-Hamilton, P.F.). Chemical toxins: a hypothesis to explain the growing obesity epidemic. Journal of Alternative and Complementary Medicine 2002;8(2):185-192.
Kim JJ, Kumar S, Kumar V, Lee YM, Kim YS, Kumar V. Bisphenols as a Legacy Pollutant, and Their Effects on Organ Vulnerability. Int J Environ Res Public Health. 2019;17(1):112. Published 2019 Dec 22. doi:10.3390/ijerph17010112
Stahlhut RW, Myers JP, Taylor JA, Nadal A, Dyer JA, Vom Saal FS. Experimental BPA Exposure and Glucose-Stimulated Insulin Response in Adult Men and Women. J Endocr Soc. 2018;2(10):1173–1187. Published 2018 Sep 12. doi:10.1210/js.2018-00151
Lehmler HJ, Liu B, Gadogbe M et al. Exposure to Bisphenol A, Bisphenol F, and Bisphenol S in U.S. Adults and Children: The National Health and Nutrition Examination Survey 2013-2014. ACS Omega 2018:3(6); 6523-6532.
vom Saal FS, Nagel SC, Coe BL, Angle BM, Taylor JA. The estrogenic endocrine disrupting chemical bisphenol A (BPA) and obesity. MolCell Endocrinol 2012;354(1–2), 74–84.
Janesick A, Blumberg B. Obesogens, stem cells and the developmental programming of obesity. IntJ Androl 2012;35(3), 437–448
Carwile JL, Michels KB. Urinary bisphenol A and obesity: NHANES 2003-2006. Environ Res. 2011;111(6):825–830. doi:10.1016/j.envres.2011.05.014
Wu W, Li M, Liu A, et al. Bisphenol A and the Risk of Obesity a Systematic Review With Meta-Analysis of the Epidemiological Evidence. Dose Response. 2020;18(2):1559325820916949. Published 2020 Apr 9. doi:10.1177/1559325820916949
Weschler CJ, et al. Transdermal uptake of diethyl phthalate and Di(n-butyl) phthalate directly from air: Experimental verification. Environ Health Perspect. 2015 Oct;123(10):928-34.
Pizzorno J. Is the Diabetes Epidemic Primarily Due to Toxins?. Integr Med (Encinitas). 2016;15(4):8–17.
Rancière F, Botton J, Slama R, et al. Exposure to Bisphenol A and Bisphenol S and Incident Type 2 Diabetes: A Case-Cohort Study in the French Cohort D.E.S.I.R. Environ Health Perspect. 2019;127(10):107013. doi:10.1289/EHP5159
Lee DH, Lee IK, Song K et al. A strong dose-response relation between serum concentrations of persistent organic pollutants and diabetes: results from the National Health and Examination Survey 1999-2002. Diabetes Care 2006 Jul;29(7): 1638-44.
Díaz Santana MV, Hankinson SE, Bigelow C, et al. Urinary concentrations of phthalate biomarkers and weight change among postmenopausal women: a prospective cohort study. Environ Health. 2019;18(1):20. Published 2019 Mar 12. doi:10.1186/s12940-019-0458-6


