Background on author
Han S Chiu, MD [email protected] www.vavici.com
Dr. Chiu is a Stanford-trained physician, venture capitalist, and former pharmaceutical executive. He is an advisor to Stanford’s Clinical Excellence Research Center and leads Malin Burnham’s San Diego based Obesity/Diabetes Working Group. He currently serves as the founder and CEO of VAVICI, a start-up seeking to pilot a root-cause-based physician platform for obesity and diabetes. What follows is an application of root-cause-based principles to challenge and improve our approach to COVID-19 policy and treatment.
Donations can be made to VAVICI FOUNDATION, a 501c3 public charity. For more information please contact Ron Bissinger at [email protected].
COVID-19: FROM CRISIS TO OPPORTUNITY –TAKING BACK OUR LIVES- PART 2 AVOIDANCE IS NOT ENOUGH
Can we really fight COVID-19 by avoiding it?
If 99% of our efforts are spent avoiding the virus,
What are we doing to fight this scourge?
And if we are to fight,
How can we get to the root of the problem?
These are just some of the questions fundamental to any root-cause-based approach to COVID-19. Social distancing and avoidance are vitally important, but they are not the same as our taking ownership to fight this crisis. Instead, the only talk we seem to have of our fighting this disease is about having someone else do so for us.
That someone is a company developing a conventional drug or vaccine, or making more ventilators or other equipment to provide supportive care.
That someone is our tireless healthcare workers who are putting their lives on the line to save us when we become seriously ill.
That someone is NOT you and me doing all we can to make ourselves healthier, our immune systems stronger, and to use the full spectrum of what we can do to fight the virus and avoid being a further burden on our healthcare system.
That someone is also NOT even the vast majority of our primary care doctors, who have not been effectively engaged in this crisis.
Counting on someone else is waiting and hoping that sometime in the future this someone will have “something” that might help us. This makes sense when there isn’t currently anything we we can do. It does not make sense when there are things we can do now, things we know will work or at least help, and which may ultimately work as well or better than this “something” we are waiting for. These things we can do now are the birds in hand that are worth far more than the ones in the bush.
The heroes who save our lives with drugs and ventilators together provide what we call sick care. It is reactive care designed for when we are already sick. It is vitally important care, which can and does save lives.
It is not, however, proactive care that by and large makes us stronger and healthier, and which strikes directly at the root causes of disease. This, in contrast, is what we might call “healthy” care, and when this “healthy” care is taken beyond traditional health and wellness to treat and reverse disease, it becomes “beyond care”.
Most of us have a general understanding of health and wellness and often believe that what we see in our company’s or health insurance plan’s wellness program is the “full spectrum” of “healthy” options. It is not. Even so, many of us have seen benefits from traditional health and wellness programs, but others have been disappointed, often citing results that are not enduring or hard to quantify and grasp. This leaves many with the impression that “healthy” care simply can’t do what drugs that treat disease do. Nothing could be further from the truth.
What we often fail to appreciate is that traditional health and wellness, while important, is not designed to treat disease. It is designed to prevent disease. Drugs in contrast are almost always used to treat disease.
Comparing a version of “healthy” care that doesn’t include treatment and saying that “healthy” care doesn’t work as well as drugs is like saying all cars are slower than horses because the only car you’ve ever know drove doesn’t have tires.
The difference becomes a lot easier to appreciate with the following cynical but candid description of the prevention encounter.
Prevention is asking someone to do something they don’t like to avoid a disease (insert name of disease) they might (or might not) get sometime in the future (usually far into the future). Where if they don’t get said disease, we can’t even say for sure that what we did worked. However, if they do get the disease, whatever we asked them to do for (insert a time frame) would have been for naught and now it’s too late to do anything different.
This isn’t to say that prevention is a bad thing. Most of what people are asked to do in the name of prevention is good (i.e. “healthy”) for them and in many situations probably will prevent disease, but the lack of certainty persists unless we actually identify, treat and reverse a disease or issue that’s present. With “beyond care” we re-introduce the idea of treatment which allows us to change the narrative to something more like…
“Beyond care” is asking someone to do something they don’t like (hard to avoid this part) to achieve a near-term measurable goal that’s meaningful (this is the essence of treatment), where if what we try doesn’t work, we quickly discard that (distasteful) intervention and try something else, thereby limiting what someone has to do to what actually works. Plus, by hitting these meaningful measurable goals, we can feel more confident that we are preventing (insert name of another disease) or we have actually treated and reversed this disease.
Can you see how “beyond care” differs from traditional health and wellness? It’s still “healthy”, but NOT the kind of health and wellness that is limited to prevention. It includes treatment.
“Beyond care” requires that we identify and treat endpoints that are measurable and meaningful enough to justify what we ask patients to do. In order to deliver these kinds of results we have to be able to utilize therapeutic approaches that go beyond traditional health and wellness, and even beyond traditional drugs and vaccines. We might use some of the same principles and even the same tools, but we would use them differently and get different results.
“Beyond care” goes beyond what traditional health and wellness programs provide by actively engaging and incorporating the insights and developments from the entire medical community. Most traditional health and wellness programs rely on a much smaller subset of the medical community to develop their methodologies, sometimes relying on a single medical institution or even a single medical study. “Beyond care” is comprehensive and collaborative.
“Beyond care” goes beyond what is available through biotech and pharmaceutical companies, which rely on a much smaller percent of the medical community (namely just the scientists working at those companies) to develop that much smaller fraction of products and technologies that is protectable by patents and amenable to FDA regulatory pathways for development.
What most of us fail to realize is that NOT all good products are patentable or even fit an FDA regulatory pathway. So, biotech and pharmaceutical company products hardly represent the “full spectrum” of what we can and should develop and use.
“Beyond care” does NOT mean we don’t use drugs and vaccines, but that we use them in the context of a more comprehensive treatment approach that focuses on root cause and not just symptoms.
If we were to draw a Venn diagram to illustrate what we are missing by focusing solely on traditional health and wellness or on solutions from biotech and pharmaceutical companies, it might look like Figure 1.
Figure 1. Venn diagram illustrating the “full spectrum” of health care options represented by Beyond Care, Traditional Health and Wellness, and Drugs and Vaccines
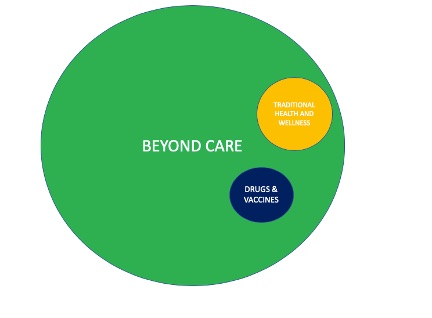
“Beyond care” opens the door to ALL legitimate evidenced based approaches including many that otherwise would never see the light of day, but yet have the ability when properly used to dramatically lower costs and improve the lives of millions. That such solutions exist and are NOT being used or even considered in our fight against COVID-19 is a national and global tragedy.
“Beyond care” means going beyond health coaches, nurses, and physician assistants to fully engage our best trained and most clinically experienced healthcare providers, our doctors.
“Beyond care” means going beyond using caregivers who know little or nothing about our healthcare issues to being able to use our own physicians who know us better than any other caregiver. Very few traditional health and wellness programs use doctors, let alone our own doctors. Worse, many seek to disintermediate them.
“Beyond care” means going beyond the much smaller pool of ER doctors and hospital physicians, to fully engage all of our 200,000 primary care physicians so they can take their proper place on the front lines against COVID-19. Most of us don’t realize that our current frontline defenders are limited to ER doctors and hospital physicians.
The much larger pool of primary care physicians is not engaged because they don’t have the proper education, tools and business model to do so effectively. If they were engaged, our health care system would not be so easily overwhelmed. When primary care physicians are engaged, the ER and our hospitals become our second and final line of defense, not the front line. That is the role ERs and hospitals are supposed to play.
If our defense against COVID-19 was like a medieval defense of a castle, primary care doctors would be the thousands of soldiers patrolling and protecting the perimeter, the gates and the walls. ER and hospital physicians would be like the much smaller number of elite guards protecting the inner sanctum, where the King and Queen would make their last stand. If the invaders breach the walls, the inner sanctum is easily overwhelmed. No King in his right mind would ever abandon all support to his soldiers in favor of making his elite guard the “front line”.
If for nearly every disease going to the ER and hospital is the LAST line of defense;
How did we let our ER and hospital physicians become the FIRST line of defense?
And then somehow wonder why our system is so easily overwhelmed.
How can we hope to fight this crisis effectively if
the vast majority of primary care doctors are NOT engaged?
How can we expect our primary care doctors to be engaged
when 99% of our COVID-19 resources DO NOT go towards helping them do so?
“Beyond care” means going beyond the knowledge of any single physician to allowing our own physician to crowd source the experiences and data from all other primary care physicians, academic physicians and the rest of the medical community. It means total collaboration which helps ensure that NO stone is unturned.
“Beyond care” means going beyond trying to cram our health and wellness into one size fits all programs. It means being able to incorporate the clinical judgement of our own physician to decide when to consider other programs and approaches and when to push and even exceed the limits of traditional guidelines. Instead of wasting precious time and energy trying all the wrong therapies in all the wrong ways, “beyond care” means being able to get the clinical judgement needed to do things right.
“Beyond care” means going beyond using vague end points and long-term (decades away) goals to identify meaningful well-defined near-term endpoints. It means going from having no idea what does and doesn’t work to knowing exactly what works and what doesn’t by using the right tests, labs and analytical tools.
To put this in perspective, I give you the case of Ms. M, an anonymized friend of mine who represents many of us. Ms. M is very health conscious and is always on top of all the latest health fads and “super” foods. She is quick to tell me about all the things she is taking to detoxify her liver, her kidneys and the rest of her body. When I ask her if it’s working, she really doesn’t know, but she is sure that these things must be good for her. Her list of supplements and interventions grows but her other health conditions don’t improve.
If the goal is detoxification, wouldn’t it make sense to do a lab test to know what we want to detoxify from and whether our intervention is working? Most health and wellness programs don’t even offer any lab testing. How many of us ever bother to get such tests? Knowing what result (lab test in this case) you need to achieve is the definition of a meaningful well-defined near-term endpoint. This is “beyond care”.
So, what happened to Ms. M?
She has now begun to work with her doctors to get the appropriate testing and to verify what works. Her health conditions are improving, and she is much happier taking fewer supplements and medicines than she was before.
Many of us believe that our doctors don’t provide “beyond care”. In most cases, we have never asked. In others, our doctors don’t have the education, the tools to deliver this education, or the proper business model to enable them to deliver this kind of care. Enabling this kind of care means supporting companies like VAVICI that seek to help both doctors and patients do their part.
“Beyond care” means shifting the focus away from waiting for someone else to fix our problems, to learning how to take primary responsibility for our own care. The only way a doctor can cost effectively provide us “beyond care” is if we do our part.
No one can do our “healthy” “beyond care” for us.
We have to own our individual health.
Avoiding and facing COVID-19 with “beyond care” are two very different, but complementary strategies.
Avoidance strives never to get exposed; “beyond care” strives to build our health so that we don’t get seriously ill when we are exposed or infected.
Avoidance provides no lasting protection and no reduction in severity of disease when we are infected. “Beyond care” helps us develop lasting protection and to reduce the severity of any illness.
Avoidance may not prevent us from getting infected, but it will “flatten the curve” so that when we do get infected our hospitals are not overwhelmed. “Beyond care” in contrast builds real protection and strives to “eliminate/reduce the curve”. It helps to create what is known as “herd immunity.”[1]
Figure 2. Flatten vs Eliminate/Reduce the curve
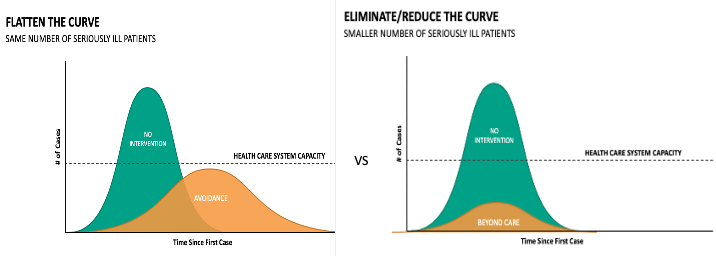
Avoidance relies on fear and panic to drive the mass compliance it requires. It shuts down the economy and instills a high level of anxiety, making even the best of us more vulnerable. “Beyond care” provides a sense of hope and control, providing concrete and constructive things we know can work.
If coronavirus were the school bully, avoidance means making sure we never run into him. Facing the problem means learning how to defend ourselves and fight for our lives. A vaccine, drug or ventilator would be like counting on a teacher to be there to protect and save us. All of these strategies are important, but not having any one of them is like going into a fight with one arm tied behind our back.
Figure 3. Avoidance vs Facing disease with traditional health and wellness and/or “Beyond care”
| Avoidance | Traditional Health and Wellness | “Beyond Care” | |
| Primary focus | Prevention | Prevention | Prevention & Treatment |
| COVID 19 curve | Flattens | Flattens | Eliminates/Reduces |
| Prevents disease | + | ++ | +++++ |
| Builds Herd Immunity | – | ++ | +++++ |
| Uses our doctor | – | – | +++++ |
| Instills hope and a sense of control | – | +++ | +++++ |
| Curative treatment potential | – | – | +++++ |
| Not one size fits all | – | – | +++++ |
| Considers new therapies and drugs | – | – | +++++ |
So just how important is it that we do our part to face this crisis?
It is critically important. Unlike past pandemics, avoidance and social distancing may not be enough. Waiting for new conventional drugs and vaccines may be too little too late.
Instead of gambling that this pandemic is a once-in-a-lifetime tragedy that will never happen again, we should be seeing this as a once-in-a-lifetime opportunity to change health care so that we are never caught off guard again.
What are the limits to our avoidance and social distancing strategy?
Most of us think of avoidance as a means to “avoid” ever getting COVID-19 at all. We believe if we wait until this all blows over, we will never be affected. While this might have been possible if we had controlled the situation early on, it is not what public health officials are promising now. What they are promising instead is that avoidance will “flatten” the curve.
So, what changed to reduce the power of avoidance?
Avoidance works best to prevent ever getting infected when the disease is relatively controllable and therefore will go away with time. It works best when infected people can be easily identified (SARS, MERS, Ebola), when very few are mildly ill or worse asymptomatic (SARS, MERS, Ebola), and when transmission is difficult (Ebola). It works best when we can limit the number of infected people. This is what we have faced with past pandemics. It is not what we are facing now.
Avoidance does not work as well to prevent us from ever getting sick when the disease is poorly controlled and there is a high number of mildly ill and asymptomatic patients. It does not work well when there are very large numbers of infected people that increase the odds for mutations and for the creation of persistent reservoirs of infection. This is the situation we currently face with the common cold and the flu, viruses that recur year after year with new and different versions. This is more like the situation we now face with COVID-19.
Figure 4. Avoidance is not enough in our current situation
| AVOIDANCE WORKS BEST WHEN | OUR CURRENT SITUATION | |
| Disease is well controlled | ++ | — |
| Infected are easily identified | ++ | — |
| Transmission is difficult | ++ | — |
| Very few are infected | ++ | — |
| Mutations are absent | ++ | — |
It’s important to understand that avoidance, when successful, does not create immunity to disease. When a disease like the Spanish Flu “burned” itself out, a substantial percentage of the population was infected to create the required “herd” immunity that prevented the disease from progressing.
An estimated 50 million died worldwide from the Spanish Flu, with over a half a million of them being Americans. By some estimates, 30 percent of the world’s population was infected before sufficient “herd” immunity was established to cause the Spanish Flu to “burn” itself out.
If 30 percent of the world’s population must be infected for COVID-19 to “burn” itself out and the death rate is 1%, then an estimated 23 million people will die worldwide, with about a million of them being from the US. Current projections for “herd” immunity to be created are 50-82% of us to be immune[2]. That’s more than double the 30% figure.
If our avoidance is effective, will we even get close to establishing the kind of “herd” immunity to “burn” COVID-19 out?
Current US projections for COVID-19 related deaths are less than one-fifth this number[3]. If so, we may not even be close to creating “herd” immunity. If we do not reach the level for effective “herd” immunity, just how much more vigilant will we have to be with screening and containment to cause COVID-19 to “burn” out, and what is the risk of a recurrence or resurgence?
Can you imagine a disease like COVID-19 returning every year?
The idea that a COVID-19-like infection might recur is not implausible. The fact that we have had SARS and MERS epidemics, which are also coronaviruses, suggests that this may already be happening.
COVID-19 is in the same family of coronaviruses that already recur every year, causing some 20% of all colds[4]. This is a family of viruses that numbers over thirty strains, of which at least five infect humans. Recurrence is possible when viruses mutate and some reservoir of infection remains. The likelihood that mutations occur, and reservoirs of asymptomatic patients exist, goes up as more people are infected. Given that this virus has already infected over a million people worldwide, it is quite possible that the thresholds for mutations and a persistent reservoir have already been met.
The potential fallout of a recurring viral infection that is more lethal than the flu is very serious. Even with an annual flu vaccine, some 20,000 to 50,000 Americans die from the flu every year. If COVID-19 remains ten times worse, it could mean losing as many as half a million American lives each year. Worse, recent statistics suggest that as many as 40% of American’s hospitalized for COVID-19 are under the age of 55[5]. With the flu, most deaths occur in the elderly who are much more easily identified and protected. Even when the young who are hospitalized do not die, the repercussions of their hospitalization for COVID-19 are serious. Many who leave the hospital are not the same. They may suffer from long term psychological trauma, lung scarring, immunosuppression and other disabilities.
Clearly, avoidance alone is not the answer.
[2] https://academic.oup.com/cid/article/52/7/911/299077
herd immunity = 1-1/R0, where R0 (a measure of infectivity). For COVID-19 R0 is estimated between 2.2 and 5.7. Therefore, herd immunity requires between 55% to 82% of the population be immune.
[3] https://www.cdc.gov/coronavirus/2019-ncov/covid-data/forecasting-us.html
[4] https://www.webmd.com/cold-and-flu/cold-guide/common_cold_causes
[5] https://www.theguardian.com/us-news/2020/apr/01/coronavirus-young-americans-covid-19

