Hospitals across the US are in critical condition. Here are 5 ways doctors are re-engaging patients, adopting new safety protocols and transitioning to new healthcare delivery models.
“A family member with cancer was supposed to have surgery. It’s been put on pause for the next couple of months because the risk of infection is too great. Cancer vs. corona?”
A friend recently shared this story. I’d asked people: Have you put off a doctor’s visit because of COVID-19? I wanted to understand how fear of the coronavirus is affecting people’s use of healthcare.
Across the US, medical procedures are being postponed. From physical exams and lab tests to diagnostic imaging and surgery.
What will be the long-term consequences for public health? How will people re-engage with the healthcare system? How should people weigh the risk of hospital-related virus exposure vs. getting the medical care they need?
To research this piece, I interviewed six doctors about how their medical practices have been affected since COVID. I spoke to other friends about their experiences getting healthcare — or making the decision to stay home and postpone medical treatment.
NOTE: This article is not meant to reflect the current state of healthcare in every part of the US, but rather to illustrate the broad challenges for patients and healthcare providers.
Here’s what I found:
- People are avoiding hospitals and clinics out of fear of exposure. Addressing patient fear will be a major challenge for healthcare systems.
- Patients with cancer, diabetes, and heart disease are particularly vulnerable.
- Telemedicine and remote patient monitoring have seen use skyrocket, but with limited effectiveness for some health conditions.
- Hospitals are losing millions of dollars a day, with potential long-term consequences for their ability to deliver high-quality care.
- Our nation’s healthcare system may look very different 1–2 years from now as a result of the coronavirus.
1. People are avoiding hospitals and clinics out of fear of Covid exposure
According to a Gallup national survey conducted in early April, more than 80% of Americans have concerns about exposure to the coronavirus in a medical facility.
Fear of COVID is causing people to skip annual physical exams. Dermatologist visits. Dentist appointments. Eye exams.
Dr. Corinna Rea, a Boston pediatrician, said: “I feel like I’m over-prescribing antibiotics for things like ear infections and strep because I can’t do exams and tests. Frustrating!”
More urgent medical conditions may be going untreated, too. Emergency room visits were down 50% last month in New York City hospitals.
“When this started, we had a massive reduction in patients showing up to the ER,” said Dr. Schehrezade Khan, an internist and hospitalist in LA. “It seemed like non-COVID related patients stopped coming to the hospital, specifically chest pain, confusion, UTI, headache.”
Dr. Ali Golshan,an LA-based interventional radiologist, said: “People are going to be scared to go to the doctor, hospital, surgery center. They will defer treatment for a while.”

Are these fears justified? It’s unclear. Not all healthcare providers seem to follow the same safety protocols.
My friend Grace wrote:
“I just walked out of the dermatologist’s office without being examined because neither he nor any of his staff were wearing masks or apparently taking any other precautions, and when I asked him how he could possibly justify this, he shrugged and said, ‘Well, nobody’s gotten sick.’ HOW CAN YOU BE A MEDICAL DOCTOR AT THIS POINT IN THE PANDEMIC AND NOT GET THAT ASYMPTOMATIC TRANSMISSION IS A THING?!?!”
Dr. Golshan noted that job losses and insurance coverage lapses may reduce people’s access to healthcare. Co-pays and out-of-pocket expenses are a challenge: “When people see their 401ks and home values go down, this makes them less likely to make any big purchases related to healthcare, as much as insurance pays for most of these procedures. This has a psychological impact.”
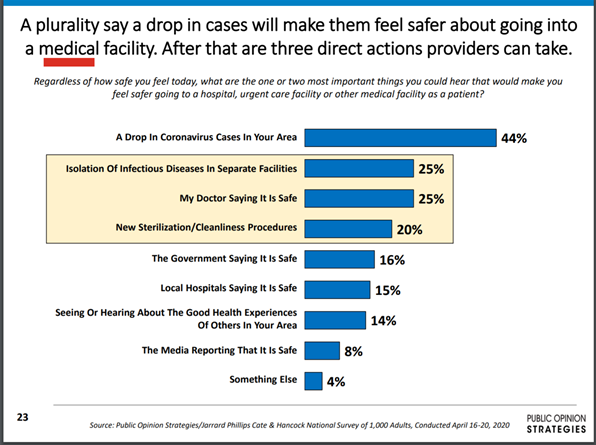
2. Addressing patient fear will be a major challenge for healthcare systems.
Healthcare organizations are developing new patient communications to show patients they’ve adopted safe new treatment protocols. Medical practices are putting up pages on their website detailing their safety protocols. They’re redesigning waiting rooms to comply with social distancing, making staff wear masks, and using temperature probes and screening questionnaires for anyone entering the hospital.
Example questions: Do you have a fever? Sore throat? Have you noticed changes to your sense of taste and smell?
Screening questions will be an important adjunct to testing. Abbott’s ID Now COVID point-of-care test can be done quickly in a health-care setting, but a recent study found it missed at least one-third of positive cases. Symptom screening will give healthcare systems a more accurate view of who poses a risk.
Healthcare systems are testing new ways to reduce the psychological barrier for patients who fear visiting a doctor. Some clinics are piloting paging systems that let patients wait in their car and have the doctor page them when they’re ready to be seen.
Reinstating visitation rights for friends and family may help rebuild patient confidence but will require improved testing availability. Healthcare facilities in some parts of the country still don’t have adequate supplies to test symptomatic patients.
To reopen successfully, healthcare systems will need to implement new treatment protocols (masks/PPE, testing, distancing) across their facilities and reassure patients they’re taking necessary safety measures.
3. Patients with cancer, diabetes, and heart disease are particularly vulnerable.
Cancer
US medical tests for detecting and monitoring cancer fell by as much as 68% in mid-March through mid-April, according to a report from Komodo Health.
Many cancer patients are deferring doctor visits, running short on prescription medications, and rationing their doses. Most individuals with cancer are immuno-compromised from both their tumors and treatments. The fear of coronavirus exposure, stopping patients from going to their hospital or clinic appointments, could lead to symptoms left unchecked and worsening of their primary conditions.
One oncologist told me:
“In addition to the lack of physical exams, cancer patients are also not undergoing their routine laboratory tests that help to guide and dictate management. These regular investigations are critically important for adverse reaction monitoring and for identifying disease progression.”
Fewer people are having important imaging studies (such as CT scans, MRIs and endoscopies). There’s concern that cancer patients may progress to more advanced stages of cancer due to lack of monitoring.
Dr. Kate Barrett, an oncology physician-specialist in LA, is the founder of Blueguide, a telemedicine service for cancer patients. Blueguide helps engage physicians with cancer patients and their family members virtually to support them in understanding their diagnosis and expanding treatment options.
Dr. Barrett wrote:
“As resources have shifted to COVID-19 care, many cancer patients have been challenged to have timely medications delivered and have received suboptimal radiotherapy schedules. A newly diagnosed lung cancer patient may have the required diagnostic procedures delayed. If their chest tumors were not removed and characterized in a critical time window, they might have spread to other areas before being targeted with the most appropriate therapy, and when they were in a much more controllable, even curable, state.”
Diabetes
More diabetes patients are using remote patient monitoring tools that provide feedback on the effects of their food intake and lifestyle on their glycemic control.Several mobile health companies offer diabetes-specific health coaching and virtual care.
However, doctors note that some diabetic emergencies are hard to spot remotely and can only be diagnosed with an in-person visit.
Heart disease
COVID fears are keeping people with serious heart symptoms away from ERs. A survey of nine major hospitals showed the number of severe heart attacks being treated in U.S hospitals had dropped by nearly 40% since March.
Dr. Dominique Kalil, a hospitalist in LA, emphasized that patients with serious conditions should not be afraid to come to the hospital:
“Patients should realize that their risk of exposure to COVID-19 in a hospital or clinic setting is far lower than the risk of an adverse or even fatal outcome of not managing chronic or even acute, progressive conditions in a timely fashion.”
Cardiologists worry about a second wave of deaths caused indirectly by COVID-19: Patients so afraid to enter hospitals that they are dying at home or waiting so long to seek care that they’re going to suffer damage to their hearts or brains.
Dr. Kalil said:
“In the past few weeks we have seen many treatable conditions evolve into irreversible situations because people delayed seeking medical care for what are usually easily managed medical issues. This has been particularly evident in cases of heart attacks and strokes, both of which, if treated early, are totally manageable, but with delays result in catastrophic long term disability.”
4. Telemedicine and remote patient monitoring have seen use skyrocket, but with limited effectiveness for some health conditions.

More physicians are conducting virtual patient visits than ever. UCSF Health Center has seen tele-visits jump from 2% to 60% in the past 2 months.
“Telemedicine has accelerated 10 years in the span of a month” said Marc Fischer, member of the Connected Health Initiative. “Medical technologists have been working for a decade to bring remote health monitoring to every home across the nation. In the span of just a few weeks since the COVID crisis, this has become reality.”
On March 17, the Department of Health and Human Services (HHS) issued new rules allowing telehealth services to be offered more broadly. The new rules allow doctors to be reimbursed for telehealth and remote patient visits at the same Medicare rate as they would for in-person visits.
The new rule lets healthcare providers use video chat applications including Apple FaceTime, Facebook Messenger video chat, Google Hangouts, Skype, and Zoom for Healthcare.
Major health plans are allowing early refills on medications before the typical 30-day requirement. Big pharmacies like CVS and Walgreens are waiving home delivery charges on prescription items.
My friend Lisa said: “I needed a prescription refill, so I booked a virtual appointment with my primary care physician two weeks ago. It took 10 minutes — so efficient. I’m wondering why this option wasn’t available earlier.”
Patients recovering from knee surgery are using digital tools for virtual physical therapy appointments. Remote heart monitoring tools from companies like AliveCor and iRhythm may help catch undiagnosed heart abnormalities in patients missing routine medical appointments.
“Telemedicine effectiveness depends on the condition,” said Dr. Rea. “I’m enjoying it for some things, and families seem to like it. But it can be hard for rashes and very exam-oriented things like ear infections.”
One friend shared her experience with telemedicine for breast cancer:
“I finished radiation treatment (breast cancer) right before COVID-19 hit. My follow up appointments were rescheduled and I’ve had 1 telemedicine appointment. It was a good check-in but the oncologist couldn’t feel or see the results. It was more a conversation which the range of “normal” is a large swing depending on the person. It was better than nothing.”
Dr. Barrett, the LA oncologist, wrote: “Several exams of cancer patients can be done via digital telehealth tools. With new medical technology, physical exams are becoming less critical to making diagnoses and managing patients.”
There are risks related to continuity of care, Dr. Barrett noted:
“It might seem hard to establish a relationship with a new doctor online. However, platforms are improving at facilitating connections and sharing information that can result in phone-into-pharmacy prescriptions. If continuity of care is broken, and patients aren’t being checked on regularly, this will have a significant impact when patients start going into doctors’ offices again.”
5. Hospitals are losing millions of dollars a day, with potential long-term consequences for their ability to deliver high-quality care.
COVID has had a devastating impact on hospitals. They’ve seen revenues flatline during the pandemic.
Many states have ordered that elective or non-urgent procedures be delayed in order to conserve PPE and free up staff and facilities for COVID-19 patients. Elective procedures include things like bariatric surgery and tonsillectomy. States have set different standards for when elective outpatient and inpatient procedures may resume.
These elective surgeries are the chief money-makers at most hospitals. Without these elective surgeries, hospitals are losing millions of dollars every day.
There’s a risk that economic ruin could throw our hospital system into as much or more chaos than treating patients.
Many hospitals under financial pressure are letting go or furloughing staff, including doctors and nurses. In some parts of the country, doctors and nurses are running out of masks and gloves. If hospitals run out of cash to buy more beds and ventilators, pay their staff or buy needed supplies, more people will die.
This is why it’s tricky reading too much into this snapshot in time. Daily hospitalization and intubation rates matter. But they’re just one piece of the puzzle. The broader question is: Will minimizing the number of COVID-19 deaths today minimize the human costs of the pandemic when the full spectrum of human consequences is considered?
Even healthcare systems that haven’t been hit hard by COVID are reserving capacity (ICU beds, ventilators, and staff). They’re preparing for a possible second wave of COVID in November/December, putting more strain on hospital capacity.
Dr. Anthony Fauci has warned that if parts of the country reopen too quickly, “there is a real risk that you will trigger an outbreak that you may not be able to control, which will set you back.”
Given these unprecedented challenges, the broader health impact of the coronavirus pandemic may not become clear for some time.
Physicians emphasize that people should not let fears of COVID exposure prevent them from seeking medical care in an emergency.
“Hospitals and clinics are doing all they can to keep patients safe from COVID-19 exposure,” said Dr. Kalil. “The risk is minimal and should never prevent anyone from seeking immediate medical care.”
If you enjoyed this article, please subscribe to my newsletter where I cover trends in health and wellness.


