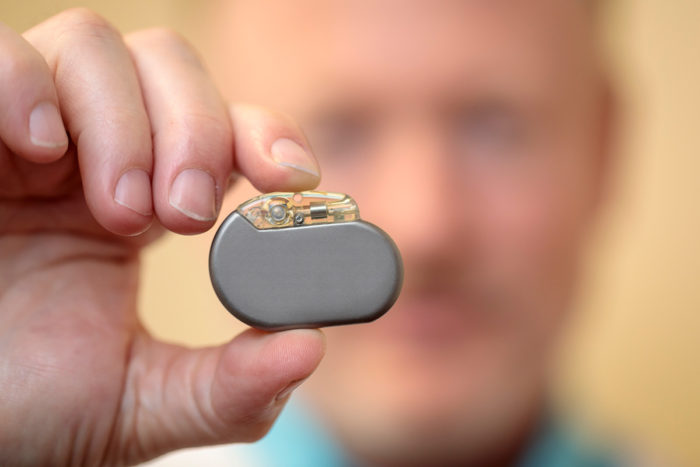
Discouraged patients see personal satisfaction improve with nerve stimultors as per, ” Charles R. Conway, MD, holds a vagus nerve stimulator as seen here on this picture. A national report driven by researchers at Washington University School of Medicine in St. Louis demonstrates that individuals treated with nerve incitement experience critical enhancements in personal satisfaction, notwithstanding when their despondency indications don’t totally scatter.”
Individuals with misery who are treated with nerve incitement experience critical enhancements in personal satisfaction, notwithstanding when their melancholy side effects don’t totally die down, as indicated by aftereffects of a national report driven by specialists at Washington University School of Medicine in St. Louis.
The investigation included about 600 patients with depression that couldn’t be alleviated by at least four antidepressants, taken either independently or in combination. The specialists assessed vagus nerve stimulators which send customary, mellow regular beats of electrical energy to the mind by means of the vagus nerve. The nerve starts in the mind, goes through the neck and goes down into the chest and midriff.
The FDA endorsed vagus nerve incitement for treatment-resistance depression in 2005, however, there has been an acknowledgment all the more as of late that assessing just a patient’s energizer reaction to incitement does not sufficiently survey the personal satisfaction, which was the reason for this examination.
The discoveries are distributed online Aug. 21 in The Journal of Clinical Psychiatry.
“While assessing patients with treatment-safe sadness, we have to concentrate more on their general prosperity,” said chief specialist Charles R. Conway, MD, a Washington University educator of psychiatry. “Many patients are on upwards of three, four or five depression prescription drugs, and they are marginally getting by. Be that as it may, when you include a vagus nerve stimulation, it truly can have a major effect in individuals’ regular daily existences.”
Upwards of 66% of the 14 million Americans with clinical depression aren’t helped by the main upper prescription medication they are recommended, and up to 33% don’t react to consequent endeavors with other such medications.
The analysts thought about patients who got vagus nerve incitement with other people who got what the examination alluded to as treatment not surprisingly, which could incorporate energizer drugs, psychotherapy, transcranial attractive incitement, electroconvulsive treatment or some blend.
The analysts pursued 328 patients embedded with the vagus nerve stimulators, a considerable lot of whom additionally took prescription drugs. They were contrasted and 271 comparatively safe depressed patients accepting just treatment obviously.
In surveying the personal satisfaction, the scientists assessed 14 classes, including physical wellbeing, family connections, the capacity to work and generally speaking wellbeing.
“On around 10 of the 14 measures, those with vagus nerve stimulators improved,” Conway said. “For an individual to be considered to have reacted to depression treatment, the person in question needs to encounter a 50 percent decrease in his or her standard misery score. In any case, we saw, narratively, that a few patients with stimulators revealed they were feeling vastly improved despite the fact that their scores were just dropping 34 to 40 percent.”
A vagus nerve stimulator is precisely embedded under the skin in the neck or chest. Incitement of the vagus nerve initially was tried in epilepsy patients who didn’t react to different medications. The FDA endorsed the device for epilepsy in 1997, however, while testing the treatment, scientists saw that some epilepsy patients who additionally had depression experienced genuinely quick enhancements in their sadness/depression indications.
In the new investigation, patients with stimulators had noteworthy gains in personal satisfaction estimates, for example, state of mind, capacity to work, social connections, family connections, and relaxation exercises, contrasted and the individuals who got just treatment of course.
Study member Charles Donovan said he never felt much better when he took stimulant medications. He was hospitalized for depression a few times before he had a stimulator embedded.
“Gradually yet definitely, my state of mind lit up,” he reviewed. “I went from being fundamentally mental to feeling next to zero sadness. I’ve had my stimulator for a long time now, regardless I get depressed when terrible things occur — like passings, retreats, work misfortune — so it doesn’t make you impenetrable from life’s ordinary good and bad times, yet for me, vagus nerve stimulator has been a distinct advantage.
“Before the stimulator, I never needed to leave my home,” he said. “It was upsetting to go to the supermarket. I couldn’t focus to sit and watch a motion picture with companions. Be that as it may, after I got the stimulator, my fixation bit by bit returned. I could do things like read a book, read the paper, watch a show on TV. Those things improved my personal satisfaction.”
Conway trusts an improved capacity to think might be vital to the advantages a few patients get from the simulator.
“It improves readiness, and that can lessen tension,” he said. “What’s more, when an individual feels progressively alarm and increasingly fiery and has a superior ability to complete a day by day schedule, nervousness and sadness levels decay.”
Conway CR, Kumar A, Xiong W, Bunker M, Aaronson ST, Rush AJ. Chronic vagus nerve stimulation significantly improves quality of life in treatment resistant major depression. The Journal of Clinical Psychiatry, published online Aug. 21, 2018.
This work was supported by LivaNova PLC (formerly Cyberonics, Inc.), the Taylor Family Institute for Innovative Psychiatry Research, the August Busch IV Foundation, and the Barnes-Jewish Hospital Foundation.
Conway previously has received research support from LivaNova and serves as a research design consultant to the company.
Washington University School of Medicine’s 1,300 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, ranking among the top 10 medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.

